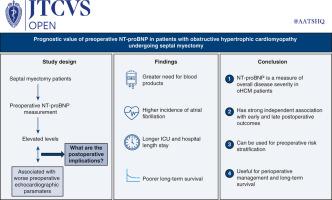
Prognostic value of preoperative NT-proBNP in patients with obstructive hypertrophic cardiomyopathy undergoing septal myectomy
IF 1.9
引用次数: 0
Abstract
Background
Proper risk stratification tools for patients with obstructive hypertrophic cardiomyopathy (oHCM) undergoing septal myectomy are lacking. Our objective was to assess the predictive value of preoperative N-terminal pro-brain natriuretic peptide (NT-proBNP) on perioperative outcomes and late survival in patients with oHCM undergoing transaortic septal myectomy.
Methods
Between 2008 and 2021, 834 patients with preoperative NT-proBNP measurements underwent septal myectomy. Restrictive cubic splines, along with multivariable logistic and Cox regression models, were used to examine the association between NT-proBNP and the outcomes. The study endpoints were early postoperative complications (postoperative atrial fibrillation, need for blood transfusion, intensive care unit [ICU] length of stay [LOS], total hospital LOS), and long-term all-cause mortality.
Results
A total of 834 patients were included in the study (median age, 58 [interquartile range (IQR), 48-65] years; 41.8% females). The median NT-proBNP concentration was 698 (IQR, 265-1446) pg/mL. Maximal septal thickness and maximal left ventricular outflow tract gradient, among other echocardiographic parameters, were linearly associated with NT-proBNP concentration (P < .001). Two patients died in the hospital (0.2%). On multivariable analysis, each 1000 pg/mL increase in NT-proBNP was independently associated with a 13% increase in blood transfusions (odds ratio, 1.13; 95% confidence interval [CI], 1.02-1.26), a 2-hour increase in ICU LOS (P < .001), and a 4-hour increase in total hospital LOS. Additionally, every 100 pg/mL increase in NT-proBNP within the range of 0 to 800 pg/mL was independently correlated with a 10% increase in the odds of postoperative atrial fibrillation. NT-proBNP also was associated with long-term mortality (hazard ratio, 1.1; 95% CI 1.04-1.14; P < .001).
Conclusions
Preoperative NT-proBNP has strong, independent associations with early and late outcomes and may be useful in stratifying, managing, and monitoring oHCM patients.
术前NT-proBNP在梗阻性肥厚性心肌病行膈肌切除术患者中的预后价值
背景梗阻性肥厚性心肌病(oHCM)行膈肌切除术的患者缺乏适当的风险分层工具。我们的目的是评估术前n端前脑利钠肽(NT-proBNP)对oHCM患者行经主动脉间隔肌切除术围手术期结局和晚期生存的预测价值。方法2008年至2021年间,834例术前NT-proBNP测量的患者接受了鼻中隔肌切除术。限制性三次样条,以及多变量逻辑和Cox回归模型,被用来检验NT-proBNP与结果之间的关系。研究终点为术后早期并发症(术后房颤、输血需求、重症监护病房(ICU)住院时间(LOS)、总住院时间(LOS))和长期全因死亡率。结果共纳入834例患者(中位年龄58岁[四分位间距48 ~ 65]岁;41.8%的女性)。NT-proBNP中位浓度为698 (IQR, 265-1446) pg/mL。在其他超声心动图参数中,最大间隔厚度和最大左心室流出道梯度与NT-proBNP浓度呈线性相关(P < .001)。2例患者在医院死亡(0.2%)。在多变量分析中,NT-proBNP每增加1000 pg/mL与输血增加13%(优势比为1.13;95%可信区间[CI]为1.02-1.26)、ICU LOS增加2小时(P < .001)和医院总LOS增加4小时独立相关。此外,在0 ~ 800 pg/mL范围内NT-proBNP每增加100 pg/mL与术后房颤发生率增加10%独立相关。NT-proBNP也与长期死亡率相关(风险比1.1;95% CI 1.04-1.14; P < .001)。结论术前NT-proBNP与早期和晚期预后有很强的独立相关性,可用于oHCM患者的分层、管理和监测。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


