Early experience with a prefabricated bioprosthetic aortic valved conduit: The first 100
IF 1.9
引用次数: 0
Abstract
Objective
To evaluate the early postoperative morbidity, mortality, and prosthetic conduit function of patients who underwent aortic root replacement using a prefabricated bioprosthetic aortic valved conduit.
Methods
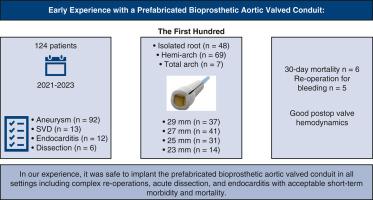
Single-center retrospective review of 124 consecutive adult patients who underwent aortic root replacement with a certified prefabricated bioprosthetic aortic valved conduit from 2021 to December 2023.
Results
Indications for operation were aortic aneurysms (n = 92), endocarditis (n = 12), deterioration of prior valve prosthesis (n = 13), and aortic dissection (n = 6). Implanted valve sizes were 29 mm (n = 37), 27 mm (n = 41), 25 mm (n = 31), 23 mm (n = 14), and 21 mm (n = 1). Isolated aortic root repair was performed in 48 patients, concomitant hemiarch in 69 patients and total arch in 7 patients. Thirty-day mortality rate was 5% (n = 6), permanent pacemaker implantation was necessary in 14% (n = 17), reoperation for bleeding in 4% (n = 5), and only 1 patient developed postoperative stroke. Discharge echocardiogram was available in 118 patients, and follow-up assessment in 45 patients. Prosthetic aortic valve gradient, effective orifice area, and Doppler velocity index remained within normal limits.
Conclusions
The prefabricated bioprosthetic aortic valved conduit was used in all settings, including complex reoperations, acute dissection, and endocarditis with acceptable short-term morbidity and mortality. The hemodynamic performance of the valve within the studied period was normal, the long-term durability and hemodynamic performance are yet to be proven.
预制生物假体主动脉瓣导管的早期经验:前100例
目的评价采用预制生物假体主动脉瓣导管进行主动脉根置换术的患者术后早期发病率、死亡率和假导管功能。方法:从2021年至2023年12月,对124例连续接受经认证的预制生物假体主动脉瓣导管主动脉根置换术的成人患者进行单中心回顾性研究。结果本组手术指征为主动脉瘤92例,心内膜炎12例,既往瓣膜置换术恶化13例,主动脉夹层6例。植入瓣膜尺寸分别为29 mm (n = 37)、27 mm (n = 41)、25 mm (n = 31)、23 mm (n = 14)和21 mm (n = 1)。孤立主动脉根部修复48例,合并出血69例,全弓7例。30天死亡率为5% (n = 6),需要植入永久性起搏器的为14% (n = 17),因出血再次手术的为4% (n = 5),只有1例患者发生术后卒中。出院超声心动图118例,随访45例。人工主动脉瓣梯度、有效孔面积、多普勒速度指数均在正常范围内。结论预制生物人工主动脉瓣导管可用于各种情况,包括复杂的再手术、急性夹层和心内膜炎,短期发病率和死亡率均可接受。研究期间瓣膜血流动力学性能正常,其长期耐久性和血流动力学性能有待证实。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


