Immunoregulatory orchestrations in osteoarthritis and mesenchymal stromal cells for therapy
IF 5.9
1区 医学
Q1 ORTHOPEDICS
引用次数: 0
Abstract
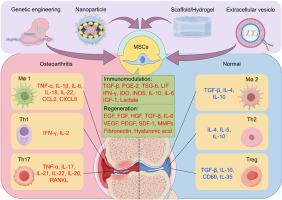
Osteoarthritis (OA) is characterized by the inability of stable and complex joint structures to function as they did, accompanied by inflammation, tissue changes, chronic pain, and neuropathic inflammation. In the past, the primary focus on the causes of joint dysfunction has been on mechanical stress leading to cartilage wear. Further researches emphasize the aging of cartilage and subchondral bone triggered cartilage lesion and osteophyte formation. Recently, the effects of immune cells, particularly macrophages and T cells, have been receiving focused attention. Herein, we primarily discuss the role of macrophages and T cells in the progression of OA and how mild inflammation in cartilage, subchondral bone, synovium, muscles, and nerves influences the progression of OA. Additionally, this review highlights the interaction between mesenchymal stromal cells (MSCs) and macrophages, as well as MSCs and T cells, along with how these interactions affect OA development and treatment. Finally, we explore future research directions and issues that still need to be addressed, providing more insights for the clinical translation of MSC-based therapy for OA.
The translational potential of this article
This review highlights the promising translational potential of MSCs in OA therapy by targeting immunoregulatory networks. MSCs directly modulating macrophage M1/M2 polarization, Th1/Th2 and Th/Treg balance of T cells to suppress inflammation, thereby promoting cartilage repair and subchondral bone remodeling. Their ability to synergize with biomaterials or drug carriers enhances therapeutic precision and efficacy. However, challenges like MSCs survival in inflammatory microenvironments, heterogeneity in immune cell responses, and personalized treatment strategies require further optimization. Advances in genetical engineered strategies, extracellular vesicles, scaffolds/hydrogels or nanoparticle-based approaches may bridge these gaps, offering scalable solutions for clinical translation. This work underscores MSC-based therapies as a transformative approach for OA, pending refinement of delivery systems and patient stratification.
骨关节炎和间充质间质细胞治疗中的免疫调节协调
骨关节炎(OA)的特点是稳定和复杂的关节结构不能正常工作,并伴有炎症、组织改变、慢性疼痛和神经性炎症。在过去,主要关注关节功能障碍的原因一直是机械应力导致软骨磨损。进一步的研究强调软骨和软骨下骨的老化引发软骨病变和骨赘的形成。近年来,免疫细胞,特别是巨噬细胞和T细胞的作用受到了人们的关注。在此,我们主要讨论巨噬细胞和T细胞在OA进展中的作用,以及软骨、软骨下骨、滑膜、肌肉和神经的轻度炎症如何影响OA进展。此外,这篇综述强调了间充质基质细胞(MSCs)和巨噬细胞之间的相互作用,以及MSCs和T细胞之间的相互作用,以及这些相互作用如何影响OA的发展和治疗。最后,我们探讨了未来的研究方向和仍需解决的问题,为骨关节炎基于msc治疗的临床转化提供更多的见解。这篇综述强调了MSCs通过靶向免疫调节网络在OA治疗中的潜在转化潜力。MSCs直接调节巨噬细胞M1/M2极化、T细胞Th1/Th2和Th/Treg平衡,抑制炎症,从而促进软骨修复和软骨下骨重塑。它们与生物材料或药物载体协同作用的能力提高了治疗精度和疗效。然而,诸如MSCs在炎症微环境中的生存、免疫细胞反应的异质性以及个性化治疗策略等挑战需要进一步优化。基因工程策略、细胞外囊泡、支架/水凝胶或基于纳米颗粒的方法的进步可能会弥补这些差距,为临床翻译提供可扩展的解决方案。这项工作强调了以骨髓间质干细胞为基础的治疗是OA的一种变革性方法,有待改进的输送系统和患者分层。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Journal of Orthopaedic Translation
Medicine-Orthopedics and Sports Medicine
CiteScore
11.80
自引率
13.60%
发文量
91
审稿时长
29 days
期刊介绍:
The Journal of Orthopaedic Translation (JOT) is the official peer-reviewed, open access journal of the Chinese Speaking Orthopaedic Society (CSOS) and the International Chinese Musculoskeletal Research Society (ICMRS). It is published quarterly, in January, April, July and October, by Elsevier.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


