Assessing coronary microvascular dysfunction in refractory no-reflow: Insights from dynamic myocardial perfusion scintigraphy and cardiac MRI
IF 2.7
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
Background
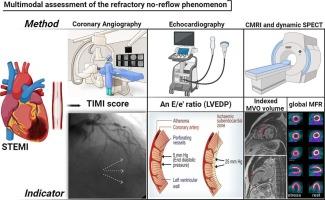
Refractory no-reflow correlates with worse outcomes, including larger infarct sizes, impaired ventricular function, and higher mortality rates, despite advances in percutaneous coronary intervention (PCI). Microvascular obstruction (MVO) and increased left ventricular end-diastolic pressure (LVEDP) are implicated in the pathogenesis, potentially exacerbating ischemic injury and limiting myocardial recovery. While pressure-wire–derived indices such as the Index of Microcirculatory Resistance (IMR) have been validated against MRI-defined MVO in STEMI populations, their invasive nature and procedural complexity limit broad adoption. In contrast, combining dynamic SPECT and cardiac MRI enables a comprehensive non-invasive functional-structural evaluation of coronary microvascular function in refractory no-reflow.
Methods
This study is a post hoc analysis of a larger randomized controlled trial (RCT) evaluating the efficacy and safety of intracoronary epinephrine in patients with refractory no-reflow post-PCI (ClinicalTrials.gov NCT04573751). We evaluated global coronary flow metrics (RMBF, SMBF, gRFI) derived from SPECT and assessed structural markers of microvascular injury (infarct size, MVO) on MRI. Echocardiographic estimations of LVEDP were also analyzed.
Results
Dynamic SPECT revealed suboptimal stress myocardial blood flow in most patients, highlighting microvascular impairment. Elevated estimated LVEDP was significantly correlated with indexed MVO (rs = 0.678, p = 0.001). Traditional flow reserve metrics showed limited sensitivity, whereas global relative flow increase (gRFI) showed a statistically significant correlation with MVO, highlighting its added value in detecting stress-induced perfusion abnormalities. Given the small sample and potential outlier influence, this observation should be considered hypothesis-generating.
Conclusion
Our findings support that functional impairments—particularly elevated LVEDP and reduced gRFI—are associated with refractory no-reflow. In particular, gRFI may serve as a promising non-invasive marker of microvascular dysfunction, complementing structural imaging. None-theless, further validation in larger cohorts is needed. This study advocates for refined multimodal imaging strategies and tailored therapeutic approaches targeting dynamic microvascular disturbances to improve outcomes in refractory no-reflow.
评估难治性非再流患者冠状动脉微血管功能障碍:来自动态心肌灌注显像和心脏MRI的见解
背景:尽管经皮冠状动脉介入治疗(PCI)技术有所进步,但难治性非再流与更糟糕的结果相关,包括更大的梗死面积、心室功能受损和更高的死亡率。微血管阻塞(MVO)和左室舒张末期压(LVEDP)升高与发病机制有关,可能加剧缺血性损伤并限制心肌恢复。虽然压力线衍生的指标,如微循环阻力指数(IMR)已经在STEMI人群中针对mri定义的MVO进行了验证,但其侵入性和程序复杂性限制了其广泛采用。相比之下,结合动态SPECT和心脏MRI可以对难治性无血流障碍患者的冠状动脉微血管功能进行全面的无创功能结构评估。方法:本研究是一项大型随机对照试验(RCT)的事后分析,该试验评估了冠状动脉内肾上腺素治疗难治性pci后无再流患者的有效性和安全性(ClinicalTrials.gov NCT04573751)。我们评估了SPECT得出的全球冠状动脉血流指标(RMBF, SMBF, gRFI),并评估了MRI上微血管损伤的结构标记(梗死面积,MVO)。超声心动图估计LVEDP也进行了分析。结果动态SPECT显示大多数患者的应激心肌血流量不理想,微血管损伤突出。估计LVEDP升高与MVO指数显著相关(rs = 0.678, p = 0.001)。传统的流量储备指标灵敏度有限,而全局相对流量增加(gRFI)与MVO的相关性具有统计学意义,突出了其在检测应力诱导的灌注异常方面的附加价值。考虑到样本小和潜在的异常值影响,这一观察结果应该被认为是假设生成。结论:我们的研究结果支持功能损伤——特别是LVEDP升高和grfi降低——与难治性无血流相关。特别是,gRFI可以作为微血管功能障碍的一种有前途的非侵入性标志物,补充结构成像。然而,需要在更大的队列中进一步验证。本研究提倡完善的多模式成像策略和针对动态微血管紊乱的量身定制的治疗方法,以改善难治性无再流的预后。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Microvascular research
医学-外周血管病
CiteScore
6.00
自引率
3.20%
发文量
158
审稿时长
43 days
期刊介绍:
Microvascular Research is dedicated to the dissemination of fundamental information related to the microvascular field. Full-length articles presenting the results of original research and brief communications are featured.
Research Areas include:
• Angiogenesis
• Biochemistry
• Bioengineering
• Biomathematics
• Biophysics
• Cancer
• Circulatory homeostasis
• Comparative physiology
• Drug delivery
• Neuropharmacology
• Microvascular pathology
• Rheology
• Tissue Engineering.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


