Risk of new onset of immune-mediated diseases after SARS-CoV-2 infection: A systematic review and meta-analysis
IF 4.4
2区 医学
Q1 RHEUMATOLOGY
引用次数: 0
Abstract
Objectives
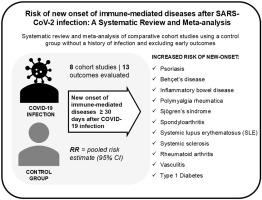
The association between SARS-CoV-2 infection and new onset of immune-mediated diseases is of interest given the conflicting evidence. This study aims to gather evidence and estimate the risk of immune-mediated diseases following SARS-CoV-2 infection.
Methods
Analytical observational studies reporting immune-mediated diseases after confirmed SARS-CoV-2 infection, compared to individuals without infection history, were included. Thirty-nine immune-mediated diseases were defined as outcomes of interest. Studies including diagnosis within the first 30 days post-infection were excluded. PubMed, EMBASE, CINAHL, Web of Science, and Europe PMC were consulted. Relative risks were pooled using a random-effects model and the Mantel-Haenszel method.
Results
Eight studies met the eligibility criteria. Meta-analyses were conducted for 13 outcomes of interest from six studies. The SARS-CoV-2 exposed group exhibited significantly higher risks for 11 conditions compared to non-exposed group: Behçet's disease, spondyloarthritis, systemic sclerosis, systemic lupus erythematosus, polymyalgia rheumatica, psoriasis, rheumatoid arthritis, Sjögren's syndrome, type 1 diabetes (in adults), vasculitis, and inflammatory bowel disease. The range of the associations varied between 2.31 (95 % CI: 1.87–2.85) for systemic sclerosis to 3.71 (95 % CI: 1.18–11.72) for Behçet's disease. Guillain-Barré syndrome and type 1 diabetes (in the paediatric population) showed no evidence of association with SARS-CoV-2 infection.
Conclusion
Our results support a higher risk of developing at least 11 immune-mediated diseases evaluated. As autoimmunity is a hallmark of post-COVID-19 syndrome, an increase in these diseases may be expected in the future. Healthcare professionals and stakeholders should prioritize research and public health surveillance based on these findings.
SARS-CoV-2感染后新发免疫介导疾病的风险:一项系统综述和荟萃分析
目的考虑到相互矛盾的证据,SARS-CoV-2感染与新发免疫介导性疾病之间的关系引起了人们的兴趣。本研究旨在收集证据并估计SARS-CoV-2感染后免疫介导性疾病的风险。方法纳入报告确诊SARS-CoV-2感染后免疫介导性疾病的分析性观察性研究,并与无感染史的个体进行比较。39种免疫介导疾病被定义为感兴趣的结果。包括感染后30天内诊断的研究被排除在外。咨询了PubMed、EMBASE、CINAHL、Web of Science和Europe PMC。使用随机效应模型和Mantel-Haenszel方法汇总相对风险。结果8项研究符合入选标准。对来自6项研究的13个相关结果进行了荟萃分析。与未暴露组相比,SARS-CoV-2暴露组在以下11种疾病中的风险明显更高:behet病、脊椎关节炎、系统性硬化症、系统性红斑狼疮、风湿性多肌痛、牛皮癣、类风湿性关节炎、Sjögren综合征、1型糖尿病(成人)、血管炎和炎症性肠病。相关性范围从系统性硬化症的2.31 (95% CI: 1.87-2.85)到behet病的3.71 (95% CI: 1.18-11.72)不等。吉兰-巴罗综合征和1型糖尿病(在儿科人群中)没有证据表明与SARS-CoV-2感染相关。结论:我们的研究结果支持至少11种免疫介导性疾病的高风险。由于自身免疫是covid -19后综合征的标志,预计未来这些疾病会增加。医疗保健专业人员和利益相关者应根据这些发现优先考虑研究和公共卫生监测。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
9.20
自引率
4.00%
发文量
176
审稿时长
46 days
期刊介绍:
Seminars in Arthritis and Rheumatism provides access to the highest-quality clinical, therapeutic and translational research about arthritis, rheumatology and musculoskeletal disorders that affect the joints and connective tissue. Each bimonthly issue includes articles giving you the latest diagnostic criteria, consensus statements, systematic reviews and meta-analyses as well as clinical and translational research studies. Read this journal for the latest groundbreaking research and to gain insights from scientists and clinicians on the management and treatment of musculoskeletal and autoimmune rheumatologic diseases. The journal is of interest to rheumatologists, orthopedic surgeons, internal medicine physicians, immunologists and specialists in bone and mineral metabolism.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


