Efficacy of thoracic paravertebral block with liposomal bupivacaine for postoperative analgesia in patients undergoing liver resection: A randomized controlled trial
IF 5.1
2区 医学
Q1 ANESTHESIOLOGY
引用次数: 0
Abstract
Background
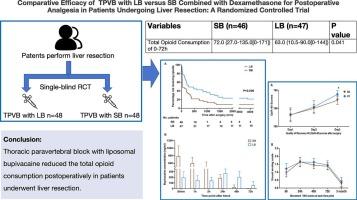
Patients often suffer from moderate to severe acute postoperative pain after liver resection, and the use of liposomal bupivacaine (LB) for pain management is widespread. However, no studies have demonstrated the effect of postoperative analgesia with LB administered via a thoracic paravertebral block (TPVB). The aim of this study was to evaluate the effects of TPVB-administered LB and standard bupivacaine (SB) on opioid sparing and postoperative recovery following liver resection
Methods
In this randomized, prospective, single-blind study, 96 patients were randomly (1:1) assigned to two groups. The primary outcome was cumulative opioid consumption over the first 72 h. the secondary outcomes were the time to first opioid use after surgery, plasma bupivacaine concentration, quality of recovery 40 (QoR-40) score area under the curve (AUC) from 24 to 72 h, pain visual analog scale (VAS) score AUC from 6 h to 3 months, postoperative plasma inflammatory factor levels, and sleep quality at 3 months after surgery
Results
Ninety-three patients (age (SD), 59.8 (10.5) years; 74 males, 79.6 %) were included in the final analysis. The cumulative opioid consumption was lower in the LB group 63.0 (IQR: 10.5, 90.0) than in the SB group of patients receiving the (72.0 (IQR: 27.0, 135.0) mg oral morphine equivalent (p = 0.041). Compared to those in the SB group, the time to first opioid use was longer, and the plasma bupivacaine and TNF-α levels were greater postoperatively in the LB group. There was no difference in other outcomes between the two groups, and there were no adverse events in this study
Conclusion
TPVB-administered LB reduced total opioid consumption postoperatively in patients undergoing hepatectomy in the first 72 h.
布比卡因脂质体胸椎旁阻滞用于肝切除术患者术后镇痛的疗效:一项随机对照试验
背景:肝切除术后患者经常出现中度至重度急性术后疼痛,布比卡因脂质体(LB)用于疼痛管理是广泛使用的。然而,没有研究证明通过胸椎旁阻滞(TPVB)给药LB术后镇痛的效果。本研究的目的是评估tpvb给药LB和标准布比卡因(SB)对肝切除术后阿片类药物节约和术后恢复的影响。方法在这项随机、前瞻性、单盲研究中,96例患者随机(1:1)分为两组。主要指标为术后72 h内阿片类药物的累计用量,次要指标为术后首次使用阿片类药物的时间、血浆布比卡因浓度、24 ~ 72 h内恢复质量(QoR-40)评分曲线下面积(AUC)、6 h ~ 3个月疼痛视觉模拟评分(VAS)评分AUC、术后3个月血浆炎症因子水平和睡眠质量。结果93例患者(年龄(SD), 59.8(10.5)岁;男性74例(79.6%)纳入最终分析。LB组患者的累计阿片类药物消耗量为63.0 (IQR: 10.5, 90.0),低于接受口服吗啡当量(72.0 (IQR: 27.0, 135.0) mg的SB组(p = 0.041)。与SB组相比,LB组首次使用阿片类药物的时间更长,术后血浆布比卡因和TNF-α水平更高。两组之间其他结局无差异,本研究未见不良事件发生。结论tpvb给药LB可减少肝切除术患者术后72小时内阿片类药物的总消耗。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
7.40
自引率
4.50%
发文量
346
审稿时长
23 days
期刊介绍:
The Journal of Clinical Anesthesia (JCA) addresses all aspects of anesthesia practice, including anesthetic administration, pharmacokinetics, preoperative and postoperative considerations, coexisting disease and other complicating factors, cost issues, and similar concerns anesthesiologists contend with daily. Exceptionally high standards of presentation and accuracy are maintained.
The core of the journal is original contributions on subjects relevant to clinical practice, and rigorously peer-reviewed. Highly respected international experts have joined together to form the Editorial Board, sharing their years of experience and clinical expertise. Specialized section editors cover the various subspecialties within the field. To keep your practical clinical skills current, the journal bridges the gap between the laboratory and the clinical practice of anesthesiology and critical care to clarify how new insights can improve daily practice.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


