Association of spinopelvic mobility and osteosarcopenia with total hip arthroplasty outcomes
Abstract
Purpose
This study assessed the association of spinopelvic mobility and osteosarcopenia with the achievement of a patient-acceptable symptom state in patient-reported outcomes after total hip arthroplasty.
Methods
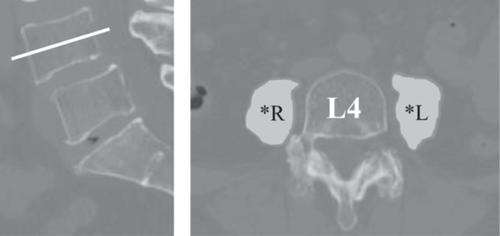
This retrospective study included 244 patients who underwent primary total hip arthroplasty with a minimum follow-up of 24 months. Spinopelvic mobility was assessed using changes in sacral slope during postural transitions, classified as stiff (<10°), normal (10°–30°), or hypermobility (≥30°). Osteosarcopenia was defined by psoas muscle area on computed tomography and lumbar bone mineral density. Outcomes were assessed using the EuroQol 5-Dimension and the Hip Disability and Osteoarthritis Outcome Score–Joint Replacement. Multivariate logistic regression analysis was performed to identify predictors of a patient-acceptable symptom state achievement on the EuroQol 5-Dimension. Propensity score matching yielded 35 patients with limited mobility and 70 controls.
Results
Physiological spinopelvic mobility (odds ratio 0.66, 95% confidence interval 0.56–0.78, p = 0.028) and the absence of osteosarcopenia (odds ratio 0.68, 95% confidence interval 0.49–0.94, p = 0.031), along with older age (odds ratio 1.12, 95% confidence interval 1.01–1.24, p = 0.046), were associated with higher patient-acceptable symptom state achievement rates for EuroQol 5-Dimension. Propensity-matched analysis revealed that patients with limited mobility exhibited significantly lower nutritional indices (p = 0.008), EuroQol 5-Dimension (p < 0.001), Hip Disability and Osteoarthritis Outcome Score–Joint Replacement (p < 0.001), and satisfaction scores (p = 0.005). Dynamic sacral slope changes correlated significantly with nutritional and muscle indices (p < 0.001).
Conclusion
Preoperative spinopelvic stiffness and osteosarcopenia independently predict poor functional recovery following total hip arthroplasty. This indicates the need for comprehensive preoperative assessments addressing both spinopelvic biomechanics and musculoskeletal health to optimise total hip arthroplasty strategies. Future research should explore tailored surgical approaches to improve outcomes in vulnerable populations, particularly those with impaired spinopelvic mobility and osteosarcopenia.
Level of Evidence
Level III, retrospective cohort study.




 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


