Rural–urban differences in health care access for postpartum parent and infant dyads
Abstract
Purpose
To examine differences in perinatal health between rural and urban postpartum parents and infants and within postpartum parent–infant dyads.
Methods
Cross-sectional analysis of the National Health Interview Survey (NHIS) data. Accounting for the complex survey design, we calculated weighted proportions of measures of self-rated health, health care utilization, and barriers to care and used chi-squared tests to assess rural–urban differences between postpartum parents and between infants, and repeated measures to test postpartum parent–infant differences within households in rural and urban counties.
Findings
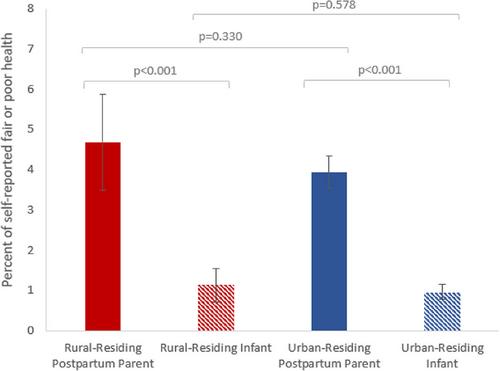
The study included 2019 rural postpartum parents, 2191 rural infants, 12,112 urban postpartum parents and 13,088 urban infants. Compared to urban postpartum parents, those living in rural areas were less likely to see an obstetrician–gynecologist (p = 0.002) had more emergency department (ED) visits (p = 0.030), reported more hospitalizations (p = 0.041), more frequently experienced uninsurance (p = 0.006), and lost Medicaid coverage after pregnancy (p = 0.006). While a higher proportion of urban infants were hospitalized than their rural counterparts (p = 0.019), other measures were similar. Accounting for dyad correlations, compared to infants, postpartum parents generally reported worse health (fair or poor self-rated health), and were more likely to experience ED visits, hospitalizations, loss of health care coverage, and barriers to care.
Conclusions
Rural postpartum parents experience worse health than their urban counterparts and compared to their infants. Rural–urban differences in access were less common among infants, thus leveraging infant care systems for services to both the infant and postpartum parent may improve household health in all communities.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


