Myeloid cell networks govern re-establishment of original immune landscapes in recurrent ovarian cancer
IF 44.5
1区 医学
Q1 CELL BIOLOGY
引用次数: 0
Abstract
Immunotherapy has shown limited success in recurrent ovarian cancer (OC), with prognostic insights largely derived from treatment-naive tumors. We analyzed 697 tumor samples (566 primary and 131 recurrent) from 595 OC patients across five independent cohorts, capturing tumor-infiltrating lymphocytes (TILs) heterogeneity and identifying four immune phenotypes linked to prognosis and TIL:myeloid networks driving malignant progression. We found that in preclinical mouse models, mirroring inflamed human OCs, the recurrent Brca1mut tumors maintained activated TILs:dendritic cells (DCs) niches but evaded immune control through upregulation of COX/PGE2 signaling. Conversely, recurrent Brca1wt tumors displayed loss of TILs:DCs niches and accumulated immunosuppressive tumor microenvironment (TME) networks featuring Trem2/ApoEhigh tumor associated macrophages (TAMs) and Nduf4l2high/Galectin3high malignant states. Recurrent tumors recapitulate the immunogenic landscapes of original cancers. Our findings reveal BRCA-dependent TIL:myeloid crosstalk as key to persistent immunogenicity in recurrent OC and propose new targets to enhance chemotherapy efficacy.

髓系细胞网络控制复发性卵巢癌原始免疫景观的重建
免疫疗法在复发性卵巢癌(OC)中显示出有限的成功,其预后见解主要来自于未经治疗的肿瘤。我们分析了来自5个独立队列的595名OC患者的697个肿瘤样本(566个原发和131个复发),捕获肿瘤浸润淋巴细胞(TIL)异质性,并确定了与预后和TIL相关的四种免疫表型:髓系网络驱动恶性进展。我们发现,在临床前小鼠模型中,与发炎的人类OCs类似,复发的Brca1mut肿瘤维持激活的TILs:树突状细胞(dc)壁龛,但通过上调COX/PGE2信号传导逃避免疫控制。相反,复发的Brca1wt肿瘤表现出TILs:DCs小生境的缺失和积累的免疫抑制肿瘤微环境(TME)网络,其特征是Trem2/ApoEhigh的肿瘤相关巨噬细胞(tam)和Nduf4l2high/ galectin - 3高的恶性状态。复发性肿瘤再现了原发肿瘤的免疫原性特征。我们的研究结果揭示了brca依赖性TIL:髓系串音是复发性OC持续免疫原性的关键,并提出了提高化疗疗效的新靶点。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
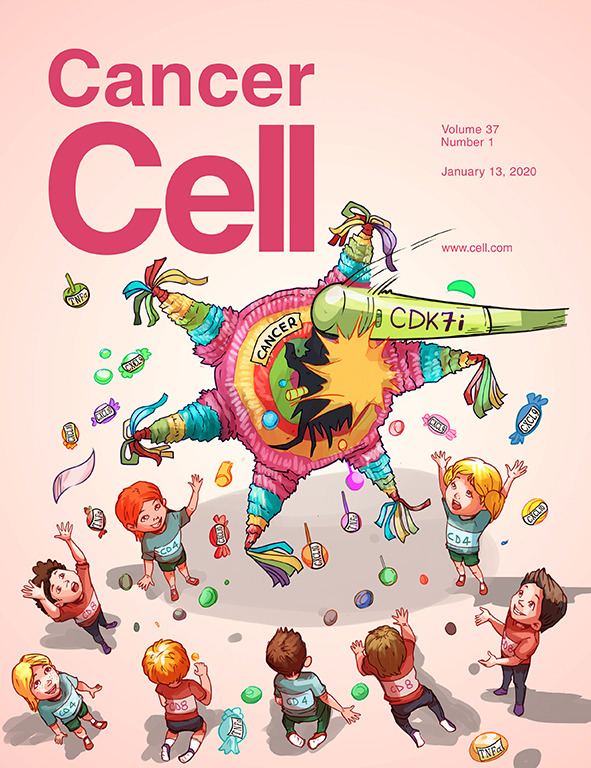
Cancer Cell
医学-肿瘤学
CiteScore
55.20
自引率
1.20%
发文量
179
审稿时长
4-8 weeks
期刊介绍:
Cancer Cell is a journal that focuses on promoting major advances in cancer research and oncology. The primary criteria for considering manuscripts are as follows:
Major advances: Manuscripts should provide significant advancements in answering important questions related to naturally occurring cancers.
Translational research: The journal welcomes translational research, which involves the application of basic scientific findings to human health and clinical practice.
Clinical investigations: Cancer Cell is interested in publishing clinical investigations that contribute to establishing new paradigms in the treatment, diagnosis, or prevention of cancers.
Insights into cancer biology: The journal values clinical investigations that provide important insights into cancer biology beyond what has been revealed by preclinical studies.
Mechanism-based proof-of-principle studies: Cancer Cell encourages the publication of mechanism-based proof-of-principle clinical studies, which demonstrate the feasibility of a specific therapeutic approach or diagnostic test.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


