Reduced Surgical Complications After Deceased-Donor Kidney Transplantation Using Inverted Allograft and Ultrashort Ureteroureterostomy: A Single-Center Experience
Abstract
Objective
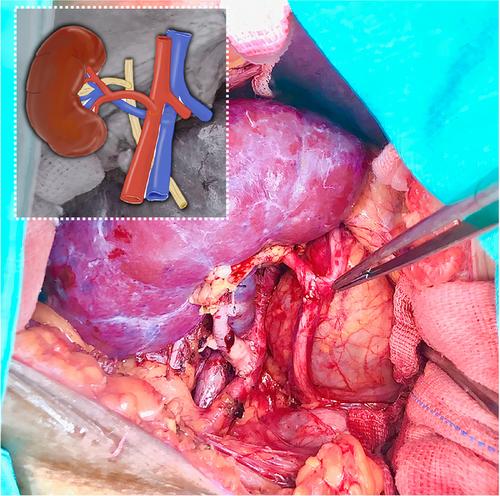
To describe the outcomes of combined inverted renal grafts and ureteroureterostomy as the primary operative approach for kidney transplantation (KTx).
Patients and Methods
This case series included adult patients who consecutively underwent deceased-donor KTx for end-stage kidney disease at our center between January 2019 and June 2022. All patients received inverted KTx combined with ultrashort anisoperistaltic end-to-side ureteroureterostomy, without ureteral stenting. Descriptive analysis focused on the major perioperative outcomes within 90 days post-transplantation.
Results
Cohort analysis of 211 patients revealed major postoperative complications requiring reoperation in 15 patients (7.11%). Reoperations for urological reasons included four patients (1.90%) with ureteral stricture and ureteral fistula in two patients each (0.95%). Ureteral strictures were managed with pyeloureterostomy, and ureteral fistulas were treated with end-to-end ureteral re-anastomosis, double-j stenting, JP drain placement, or pyeloureterostomy. Non-urological complications leading to reoperation included peri-graft collections and infections such as surgical hematoma (1.42%), deep surgical infection (1.90%), and wound dehiscence (1.90%). Three patients (1.42%) ultimately underwent transplantectomy because of graft loss after severe infection in two patients (0.95%) and acute rejection plus infection in one patient (0.47%). All the remaining patients were treated with surgical exploration, evacuation/irrigation, and wound closure. Vascular complications occurred in one patient with an arterial stricture (0.47%). Delayed graft function was found in 82.9% of the patients, with 95.26% achieving resolution within 4 weeks post-transplantation.
Conclusions
Inverted KTx combined with ultrashort end-to-side ureteroureterostomy is a feasible and safe technique with low rates of urological and vascular complications in our experience. To our knowledge, this is the largest case series using this combined surgical approach as the primary technique for deceased-donor KTxs.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


