Incidence of kidney toxicity of non-steroidal anti-inflammatory drugs in critically ill patients
IF 2.9
3区 医学
Q2 CRITICAL CARE MEDICINE
引用次数: 0
Abstract
Background
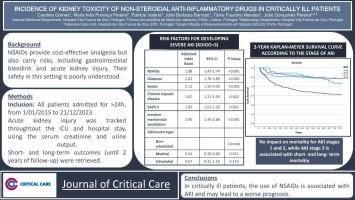
Analgesia is paramount to improving critically ill patients recovery and preventing complications, especially during the post-operative time. Nonsteroidal anti-inflammatory drugs (NSAIDs) provide cost-effective analgesia but also carry risks, including gastrointestinal bleeding and acute kidney injury (AKI). Their safety in this setting is poorly understood.
Methods
All patients admitted to the Hospital Vila Franca de Xira ICU for more than 24 h, from January 1st 2015, to December 31st 2023, were included. Acute kidney injury was tracked throughout the ICU and hospital stay for all included patients, using the serum creatinine and urine output. Patients already with kidney dysfunction on admission to the ICU, either chronic or acute, were excluded. Short- and long-term outcomes (until 2 years of follow-up) were retrieved.
Results
The study included 1157 patients. NSAIDs were more commonly used among surgical patients (62. in non-scheduled and 61. in scheduled surgery) than medical patients (23., p < 0.001). Its use was associated with higher AKI rates (67. vs. 51., p = 0.009), including severe AKI (stage 3, 34. vs. 26., p = 0.008). Notably, while non-severe AKI had no significant impact on 2-year survival, severe AKI was associated with significantly worse survival (adjusted hazard ratio 1.42, confidence interval 1.09–1.86, p = 0.011). Recovery of renal function did not significantly decrease the long-term survival (80. vs. 78., log-rank test, p = 0.636).
Conclusion
In critically ill patients, the use of NSAIDs is associated with AKI and may lead to a worse prognosis.
危重患者非甾体类抗炎药肾毒性的发生率
背景:镇痛对于提高危重病人的康复和预防并发症至关重要,尤其是在术后。非甾体抗炎药(NSAIDs)提供了具有成本效益的镇痛药,但也有风险,包括胃肠道出血和急性肾损伤(AKI)。人们对他们在这种环境下的安全性知之甚少。方法选取2015年1月1日至2023年12月31日在西维拉法兰西医院ICU住院24 h以上的患者。使用血清肌酐和尿量对所有纳入的患者在ICU和住院期间的急性肾损伤进行跟踪。在ICU入院时已经有肾功能障碍的患者,无论是慢性还是急性,均被排除在外。检索了短期和长期结果(直到2年随访)。结果共纳入1157例患者。非甾体抗炎药更常用于外科患者(62。不定期航班和61号航班。在预定手术中)比内科患者(23。, p &;0.001)。它的使用与较高的AKI发生率相关(67。与51。, p = 0.009),包括重度AKI(3期,34期)。与26。, p = 0.008)。值得注意的是,虽然非严重AKI对2年生存率无显著影响,但严重AKI与明显较差的生存率相关(校正风险比1.42,置信区间1.09-1.86,p = 0.011)。肾功能恢复没有显著降低长期生存率(80。与78年。, log-rank检验,p = 0.636)。结论危重患者使用非甾体抗炎药与急性肾损伤相关,且预后较差。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of critical care
医学-危重病医学
CiteScore
8.60
自引率
2.70%
发文量
237
审稿时长
23 days
期刊介绍:
The Journal of Critical Care, the official publication of the World Federation of Societies of Intensive and Critical Care Medicine (WFSICCM), is a leading international, peer-reviewed journal providing original research, review articles, tutorials, and invited articles for physicians and allied health professionals involved in treating the critically ill. The Journal aims to improve patient care by furthering understanding of health systems research and its integration into clinical practice.
The Journal will include articles which discuss:
All aspects of health services research in critical care
System based practice in anesthesiology, perioperative and critical care medicine
The interface between anesthesiology, critical care medicine and pain
Integrating intraoperative management in preparation for postoperative critical care management and recovery
Optimizing patient management, i.e., exploring the interface between evidence-based principles or clinical insight into management and care of complex patients
The team approach in the OR and ICU
System-based research
Medical ethics
Technology in medicine
Seminars discussing current, state of the art, and sometimes controversial topics in anesthesiology, critical care medicine, and professional education
Residency Education.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


