Steatosis non-invasive tests accurately predict metabolic dysfunction-associated steatotic liver disease, while fibrosis non-invasive tests fall short: Validation in U.S. adult population
IF 2.4
4区 医学
Q2 GASTROENTEROLOGY & HEPATOLOGY
Clinics and research in hepatology and gastroenterology
Pub Date : 2025-07-01
DOI:10.1016/j.clinre.2025.102649
引用次数: 0
Abstract
Introduction
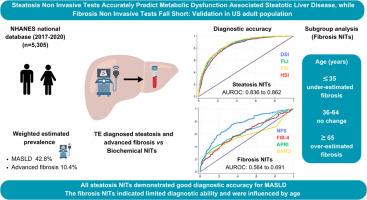
Metabolic dysfunction associated steatotic liver disease (MASLD) has replaced NAFLD as the diagnostic standard. This study aimed to validate non-invasive tests (NITs) for hepatic steatosis and fibrosis, originally used for NAFLD, in predicting MASLD and advanced fibrosis, respectively, compared to transient elastography (TE).
Methods
This cross-sectional study used the NHANES database (2017–2020). Adults aged ≥18 years with valid TE status and without other steatotic liver diseases were included. Hepatic steatosis NITs were compared against controlled attenuation parameter (CAP)- diagnosed MASLD and fibrosis NITS were compared against liver stiffness measurement (LSM)-diagnosed advanced fibrosis. The diagnostic accuracy was assessed using weighted ROC analysis.
Results
Among 5305 participants (49.1 % males), MASLD prevalence was 42.8 % (CAP-diagnosed) and advanced fibrosis was identified in 10.4 % (LSM-diagnosed) in those with MASLD. Steatosis NITs showed good diagnostic accuracy for predicting MASLD (AUROC 0.836 to 0.862), with fatty liver index having the maximum Youden index (0.55). Fibrosis NITs indicated poor to fair diagnostic accuracy for predicting advanced fibrosis (AUROC 0.564 to 0.691) but indicated high negative predicted value (89 %-94 %). In age categorized subgroup analysis, fibrosis NITs performed poorly in those aged ≤ 35 years and had low specificity to exclude fibrosis in those aged ≥65 years but performed comparably to the overall MASLD cohort in those aged 36–64 years.
Conclusion
In this population-based cohort of U.S. adults, all steatosis NITs demonstrated good diagnostic accuracy for MASLD. However, the fibrosis NITs showed limited diagnostic ability and were influenced by age, suggesting they should be used cautiously in general population.
脂肪变性非侵入性试验准确预测代谢功能障碍相关的脂肪变性肝病,而纤维化非侵入性试验不足:在美国成年人中的验证
代谢功能障碍相关脂肪变性肝病(MASLD)已取代NAFLD成为诊断标准。与瞬时弹性成像(TE)相比,本研究旨在验证肝脂肪变性和肝纤维化的无创试验(NITs)在预测MASLD和晚期纤维化方面的作用,NITs最初用于NAFLD。方法:本横断面研究使用NHANES数据库(2017-2020)。年龄≥18岁、有效TE状态且无其他脂肪变性肝脏疾病的成年人纳入研究。将肝脂肪变性NITs与控制衰减参数(CAP)诊断的MASLD进行比较,将纤维化NITs与肝刚度测量(LSM)诊断的晚期纤维化进行比较。采用加权ROC分析评估诊断准确性。结果:在5305名参与者中(49.1%男性),MASLD患病率为42.8% (cap诊断),在MASLD患者中,10.4% (lsm诊断)确诊为晚期纤维化。脂肪变性NITs对预测MASLD具有较好的诊断准确性(AUROC为0.836 ~ 0.862),其中脂肪肝指数约登指数最高(0.55)。纤维化NITs显示预测晚期纤维化的诊断准确性较差(AUROC为0.564 ~ 0.691),但显示较高的阴性预测值(89% ~ 94%)。在年龄分类亚组分析中,纤维化NITs在年龄≤35岁的人群中表现不佳,在年龄≥65岁的人群中排除纤维化的特异性较低,但在36-64岁的人群中与整体MASLD队列的表现相当。结论:在这个以人群为基础的美国成年人队列中,所有脂肪变性nit对MASLD的诊断都具有良好的准确性。然而,纤维化NITs的诊断能力有限,且受年龄的影响,提示在普通人群中应谨慎使用。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Clinics and research in hepatology and gastroenterology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
4.30
自引率
3.70%
发文量
198
审稿时长
42 days
期刊介绍:
Clinics and Research in Hepatology and Gastroenterology publishes high-quality original research papers in the field of hepatology and gastroenterology. The editors put the accent on rapid communication of new research and clinical developments and so called "hot topic" issues. Following a clear Editorial line, besides original articles and case reports, each issue features editorials, commentaries and reviews. The journal encourages research and discussion between all those involved in the specialty on an international level. All articles are peer reviewed by international experts, the articles in press are online and indexed in the international databases (Current Contents, Pubmed, Scopus, Science Direct).
Clinics and Research in Hepatology and Gastroenterology is a subscription journal (with optional open access), which allows you to publish your research without any cost to you (unless you proactively chose the open access option). Your article will be available to all researchers around the globe whose institution has a subscription to the journal.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


