Use of obesity medications in a young pediatric patient with optic nerve hypoplasia and severe early-onset obesity: A case report
引用次数: 0
Abstract
Introduction
Pediatric obesity presents complex challenges in children with underlying endocrine disorders. In patients with optic nerve hypoplasia (ONH) and hypothalamic-pituitary dysfunction, lifestyle changes alone are often ineffective for obesity treatment. This case report describes targeted pharmacologic interventions for severe early-onset obesity in a child with ONH and multiple pituitary hormone deficiencies.
Case presentation
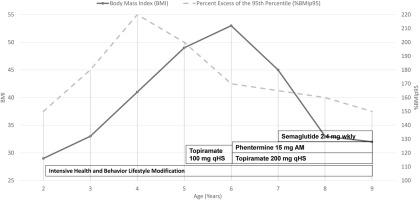
A Hispanic female was diagnosed at 45 days of life with ONH and central arginine vasopressin deficiency, central hypothyroidism, secondary adrenal insufficiency, and growth hormone deficiency. Despite early interventions, her weight-for-length percentile rose from the 65th to >97th by nine months, with continued acceleration to body mass index (BMI) of 52 kg/m2 by age 5. Topiramate 100 mg nightly was initiated, with some associated appetite suppression and weight deceleration appreciated. Weight continued to increase during the COVID-19 pandemic, and at age 6, the dose of topiramate was increased (200 mg nightly) and phentermine 15 mg daily was added. An 11 % BMI reduction was observed over the subsequent 12 months, leading to BMI of 47 kg/m2 at age 7. Due to persistent and worsening obstructive sleep apnea (OSA) despite BMI reduction, semaglutide was then initiated, with ramp-up to 2.4 mg weekly, resulting in BMI reduction of 30 % over 24 months with triple-agent therapy, and associated resolution of OSA, elevated liver enzymes, and hypertriglyceridemia.
Discussion
This case highlights the potential role and therapeutic benefit of early, targeted pharmacologic intervention in managing severe obesity in pediatric patients with hypothalamic dysfunction and ONH. In a setting where lifestyle modifications alone are insufficient, the use of combination obesity medications resulted in substantial and sustained BMI reduction, alongside resolution of obesity-related comorbidities. These findings underscore the need for proactive, individualized treatment strategies in complex pediatric obesity.
在视神经发育不全和严重早发性肥胖的年轻儿童患者中使用减肥药:1例报告
儿童肥胖对伴有潜在内分泌紊乱的儿童提出了复杂的挑战。对于视神经发育不全(ONH)和下丘脑-垂体功能障碍的患者,仅仅改变生活方式往往对肥胖治疗无效。本病例报告描述了针对患有ONH和多种垂体激素缺乏的儿童的严重早发性肥胖的靶向药物干预。病例介绍:一名西班牙裔女性在出生45天时被诊断为ONH和中枢性精氨酸抗利尿激素缺乏、中枢性甲状腺功能减退、继发性肾上腺功能不全和生长激素缺乏。尽管早期干预,她的身高体重百分位数在9个月时从第65位上升到第97位,到5岁时体重指数(BMI)继续加速到52 kg/m2。托吡酯100mg每晚开始,有一些相关的食欲抑制和体重减轻。在COVID-19大流行期间,体重继续增加,在6岁时,托吡酯剂量增加(每晚200 mg),芬特明每天添加15 mg。在随后的12个月里,观察到BMI下降了11%,导致7岁时BMI为47 kg/m2。尽管BMI降低,但由于阻塞性睡眠呼吸暂停(OSA)持续恶化,随后开始使用西马鲁肽,每周增加2.4 mg,导致在三药治疗的24个月内BMI降低30%,并相关解决OSA,肝酶升高和高甘油三酯血症。本病例强调了早期、有针对性的药物干预在治疗伴有下丘脑功能障碍和ONH的儿童严重肥胖患者中的潜在作用和治疗益处。在仅仅改变生活方式是不够的情况下,联合使用减肥药可以显著和持续地降低BMI,同时解决与肥胖相关的合并症。这些发现强调了在复杂的儿童肥胖中需要积极的、个性化的治疗策略。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


