Solid Medication Intake in Hospitalised Patients With Dysphagia: A Challenge for Speech and Language Pathologists?
Abstract
Purpose
Speech and language pathologists (SLP) are frequently consulted for guidance on the management of oral solid medications. However, the extent to which SLPs consider solid medication intake during swallowing examination remains unclear. The present study endeavoured to find out whether and how SLPs assess patients’ ability to swallow solid dosage forms (SDF) in clinical settings, with a specific focus on stroke units.
Methods
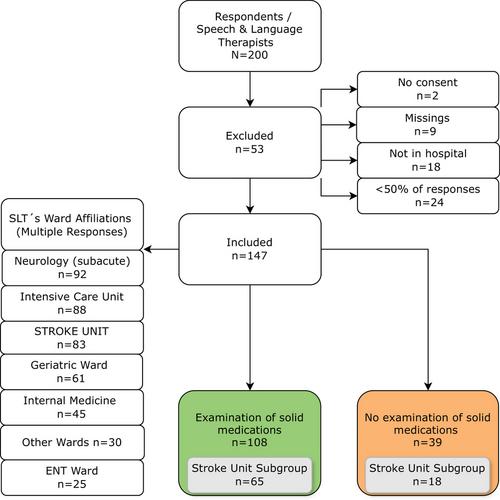
An online cross-sectional survey was conducted among SLPs in German-speaking countries. The questionnaire was targeted at SLPs working in hospitals and distributed through both direct outreach and passive dissemination on social networks.
Results
Of 200 returned questionnaires, 147 were eligible for inclusion. Of these, 108 (73.5%) evaluated the swallowing ability of solid oral medications and were further analysed. During clinical swallowing examination, the patient's own medication is most frequently used (63.9%). 92.6% of the 108 SLPs stated that they regularly offer guidance on altering SDFs. SLPs' decision to recommend modified SDFs or pause them is influenced by oral cavity retention of SDFs, pharyngeal phase disorders and SDF intake-related coughing. Additionally, SLPs employ textures that were determined to be safe for accompanying boluses, with fruit puree and water being the most preferred types. Responses of SLPs working on stroke units did not differ significantly from those working on other wards.
Conclusion
SLPs commonly evaluate the swallowing ability of SDFs. Typically, they utilise the patient's own medications for testing purposes and previously trialled consistencies as accompanying boluses. Specific evaluation and educational programs are needed to enhance the management quality of oral SDFs.
Trial Registration: ClinicalTrials.gov identifier: Registration ID: NCT05173051/Protocol ID: 11TS003721
WHAT THIS PAPER ADDS
- Speech Language Pathologists are crucial in assessing and managing dysphagia. Recent studies and guidelines suggest that it is important for SLPs to evaluate the ability to swallow solid medications. However, there is limited research on whether and how SLPs assess and manage solid dosage forms in patients with dysphagia, especially those with post-stroke dysphagia. Although a few studies have used instrumental assessments like FEES to evaluate pill swallowing, there is a lack of standardised methods.
- The findings indicate that almost three-quarters of the surveyed SLPs do evaluate SDFs, with fruit puree and water being the most preferred accompanying boluses. Patients' own medications are more frequently used in clinical swallowing examinations (CSE), whilst placebos are preferred in instrumental assessments. A large majority of SLPs are involved in deciding whether solid medications should be modified for patients with dysphagia.
- The research highlights the need for standardised protocols for the evaluation of swallowing SDFs as part of both clinical and instrumental assessments. Additionally, there is a critical need for the establishment of professional and regulatory guidelines to ensure consistent and evidence-based practices among SLPs, potentially improving patient care and medication administration.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


