Limited awareness and use of HIV post-exposure prophylaxis among people vulnerable to HIV acquisition in Western Kenya: a cross-sectional analysis
Abstract
Introduction
HIV post-exposure prophylaxis (PEP) can prevent HIV acquisition and facilitates linkage to pre-exposure prophylaxis (PrEP) for people with ongoing vulnerability. We assessed PEP awareness and use in Western Kenya.
Methods
We used cross-sectional screening/enrolment data from the Multinational Observational Cohort of HIV and other Infections (MOCHI) study. Eligible participants had behavioural vulnerability to HIV and were ages 14–55 years. Participants completed questionnaires on demographics, sexual/behavioural history, and PEP/PrEP awareness and use. Depression was assessed using the Patient Health Questionnaire (PHQ-9) with none/minimal, mild and moderate/severe depression defined as PHQ-9 scores of 0–4, 5–9 and ≥10, respectively. We used multivariable robust Poisson regression with purposeful variable selection to estimate adjusted prevalence ratios (aPRs) and 95% confidence intervals (CIs) for factors associated with PEP awareness.
Results
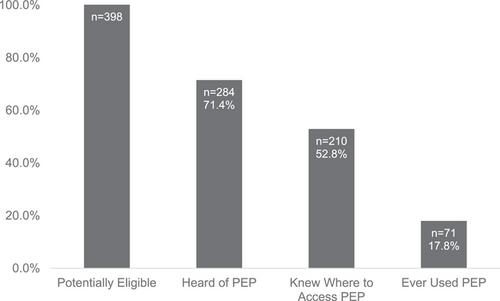
From December 2021 to May 2023, 398 participants indicated whether they heard of PEP. The median age was 22 years (IQR 19–24), 316/399 (79.2%) were female and 315/389 (81.0%) reported sex work or transactional sex. One hundred fourteen (28.6%) participants had never heard of PEP, of whom 79 (69.3%) had also not heard of PrEP. Among 284 participants who had heard of PEP, 74 (26.1%) did not know where to access it. Seventy-one participants (17.8%) had taken PEP, of whom 17 (23.9%) encountered problems accessing PEP such as unavailability (n = 5) or prohibitive expense (n = 4). In the final model, only <12 years of education (aPR 1.65 [95% CI 1.16–2.34]) and not cohabitating (aPR 2.81 [95% CI = 1.11–7.08]) were associated with never having heard of PEP. Among participants who had heard of PEP, factors associated with not knowing where to access PEP were <12 years of education (aPR 2.20 [95% CI 1.37–3.54]) and depression (mild aPR 1.86 [95% CI 1.17–2.96]; moderate/severe aPR 1.84 [95% CI 1.09–3.09], compared to none/minimal).
Conclusions
Despite enrolling a behaviourally vulnerable group potentially eligible for PEP, we identified substantial gaps in PEP awareness, access and use. Demand generation and improved access to PEP are needed to maximize the impact on reducing HIV incidence. Interventions to improve PEP awareness and access may be most impactful for people with lower education or when coupled with mental health services.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


