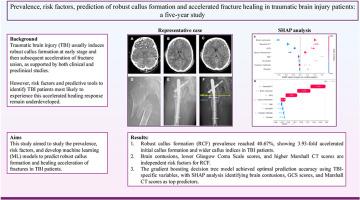
Prevalence, risk factors, prediction of robust callus formation and accelerated fracture healing in traumatic brain injury patients: a five-year study
IF 5.9
1区 医学
Q1 ORTHOPEDICS
引用次数: 0
Abstract
Background
Traumatic brain injury (TBI) usually induces robust callus formation at early stage and then subsequent acceleration of fracture union, as supported by both clinical and preclinical studies. However, risk factors and predictive tools to identify TBI patients most likely to experience this accelerated healing response are lacking and subject to future development.This study aimed to study the prevalence, risk factors, and develop machine learning (ML) models to predict robust callus formation and healing acceleration of fractures in TBI patients.
Methods
Between January 2018 and 2023, patients sustaining concomitant TBI and diaphyseal fractures who were admitted into the First Affiliated Hospital of Shantou University Medical College were evaluated retrospectively. The TBI patients were categorized into robust callus formation group (RCF) and normal callus formation group (NCF) based on follow-up radiographic fracture callus index assessments. Risk factors for RCF occurrence were first identified using traditional univariate and multivariate regression model, and predictive models were developed using 12 ML models (including traditional logistic regression model). The performance and interpretations of ML models were evaluated using the area under the receiver operating characteristic curve (AUC) and Shapley Additive Explanations (SHAP).
Results
Of the 723 patients reviewed, 150 cases were enrolled for final analysis. The prevalence of robust callus formation was 40.67 % (61/150) with significantly wider callus index (2.01 ± 0.61 vs 1.17 ± 0.12, P < 0.001) and acceleration in time to initial callus formation (22.92 ± 11.98 days vs 90.18 ± 34.52 days, P < 0.001). Brain contusions (OR 5.914, 95 % CI:2.479–14.108,P < 0.001), greater TBI severity levels evaluated using Glasgow Coma Scale (GCS, OR 3.074, 95 % CI:1.149–8.222,P = 0.025) and Marshall CT classifications (OR 2.845, 95 %CI:1.095–7.390,P = 0.032) were identified as independent risk factors for RCF occurrence. The gradient boosting decision tree (GBDT) algorithm demonstrated optimal predictive performance using TBI-specific variables, achieving an AUC of 0.86 ± 0.03. SHAP analysis revealed brain contusion, GCS scores, and Marshall CT classification scores as the three most influential clinical features.
Conclusions
For the first time, this study provided the prevalence and risk factors contributing to RCF occurrence in TBI patients with combined diaphyseal fractures, and also developed ML models for its prediction, for which it may optimize orthopedics treatment strategies and decision making in these unique set of TBI patients.
The translational potential of this article
The findings from this study offer crucial insights to enhance clinical decision-making and treatment approaches for managing fractures in TBI patients. Furthermore, our research establishes a groundwork for future investigations into the mechanisms linking TBI and enhanced osteogenesis, potentially aiding in addressing intricate bone regeneration obstacles like non-unions and critical-size defects.
外伤性脑损伤患者的患病率、危险因素、强健骨痂形成和骨折加速愈合的预测:一项为期五年的研究
临床和临床前研究都支持创伤性脑损伤(TBI)通常在早期诱导强健的骨痂形成,随后加速骨折愈合。然而,识别最有可能经历这种加速愈合反应的TBI患者的风险因素和预测工具尚缺乏,并有待于未来的发展。本研究旨在研究创伤性脑损伤患者骨折的患病率、危险因素,并开发机器学习(ML)模型来预测强健的骨痂形成和骨折愈合加速。方法回顾性分析2018年1月至2023年1月汕头大学医学院第一附属医院收治的脑外伤合并骨干骨折患者的临床资料。根据随访骨折骨痂指数评估,将TBI患者分为强健骨痂形成组(RCF)和正常骨痂形成组(NCF)。首先采用传统的单因素和多因素回归模型确定RCF发生的危险因素,并采用12 ML模型(包括传统的logistic回归模型)建立预测模型。使用接受者工作特征曲线下面积(AUC)和Shapley加性解释(SHAP)来评估ML模型的性能和解释。结果在723例患者中,150例纳入最终分析。愈伤组织形成率为40.67%(61/150),愈伤组织指数显著增大(2.01±0.61 vs 1.17±0.12,P <;0.001)和愈伤组织形成时间加速(22.92±11.98天vs 90.18±34.52天),P <;0.001)。脑挫伤(OR 5.914, 95% CI: 2.479-14.108,P <;0.001),使用格拉斯哥昏迷量表(GCS, OR 3.074, 95% CI: 1.149-8.222,P = 0.025)和Marshall CT分类(OR 2.845, 95% CI: 1.095-7.390,P = 0.032)评估的较大TBI严重程度被确定为RCF发生的独立危险因素。梯度增强决策树(GBDT)算法在使用tbi特定变量时表现出最佳的预测性能,AUC为0.86±0.03。SHAP分析显示脑挫伤、GCS评分和Marshall CT分类评分是三个最具影响的临床特征。结论本研究首次提供了颅脑损伤合并骨干骨折患者发生RCF的患病率和危险因素,并建立了预测RCF的ML模型,为这类独特的颅脑损伤患者优化骨科治疗策略和决策提供了依据。本研究的发现为加强创伤性脑损伤患者骨折的临床决策和治疗方法提供了重要的见解。此外,我们的研究为进一步研究创伤性脑损伤与增强成骨的机制奠定了基础,可能有助于解决复杂的骨再生障碍,如骨不连和临界尺寸缺陷。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Journal of Orthopaedic Translation
Medicine-Orthopedics and Sports Medicine
CiteScore
11.80
自引率
13.60%
发文量
91
审稿时长
29 days
期刊介绍:
The Journal of Orthopaedic Translation (JOT) is the official peer-reviewed, open access journal of the Chinese Speaking Orthopaedic Society (CSOS) and the International Chinese Musculoskeletal Research Society (ICMRS). It is published quarterly, in January, April, July and October, by Elsevier.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


