Atrial Fibrillation Is Associated With Increased In-Hospital and 1-Year Mortality in Patients Receiving Hemodialysis With ST Elevation Myocardial Infarction: A Retrospective Cohort Study
IF 3.4
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
Abstract
Rationale & Objective
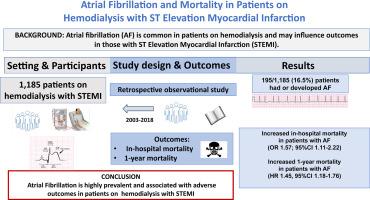
Atrial fibrillation (AF) is highly prevalent among patients receiving maintenance hemodialysis (HD) and patients with ST elevation myocardial infarction (STEMI). We investigated the association of AF with in-hospital mortality, 1-year mortality, and 1-year readmission for acute myocardial infarction (AMI) in HD patients admitted with STEMI.
Study Design
Retrospective cohort study based on a large administrative database.
Setting & Participants
138,939 patients admitted with STEMI from 2003-2018, of whom 1,185 (8.5%)receiving HD, followed from the date of admission until death, migration, or 1 year after discharge.
Exposures
STEMI (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] 410.x) as the primary discharge diagnosis, maintenance HD (ICD-9-CM 39.95; 54.98; V560; V563.1; V563.2), and AF (ICD-9-CM 427.31).
Outcomes
In-hospital all-cause mortality (primary outcome), 1-year all-cause mortality, and 1-year readmission for AMI (secondary outcomes).
Analytical Approach
Multivariable logistic regression and multivariable Cox regression.
Results
One hundred and ninety-five out of 1,185 (16.5%) patients had AF at admission or developed AF during hospitalization. After adjusting for possible confounders, AF versus sinus rhythm was associated with higher in-hospital mortality (odds ratio [OR] = 1.57; 95% confidence interval [CI], 1.11-2.22). AF was associated with higher 1-year mortality (hazard ratio [HR] = 1.45; 95% CI, 1.18-1.76), whereas it was not associated with higher 1-year readmission for AMI (HR = 1.05; 95% CI, 0.72-1.53). Less than 20% of patients with AF discharged alive were prescribed oral anticoagulant therapy. In this subgroup, oral anticoagulant therapy was associated with lower 1-year mortality (HR = 0.46; 95% CI, 0.24-0.89).
Limitations
Potential bias due to incorrect or incomplete coding, retrospective design, incidence of thromboembolic events after discharge, and cause of 1-year mortality unknown.
Conclusions
AF is highly prevalent and associated with adverse short- and long-term outcomes in HD patients admitted with STEMI.
Plain-Language Summary
Atrial fibrillation (AF) is common both in patients with kidney failure receiving hemodialysis (HD) and in those with acute myocardial infarction. We investigated retrospectively the impact of AF on 1,185 patients receiving HD admitted for ST elevation myocardial infarction (STEMI). We examined the incidence of in-hospital mortality, 1-year mortality, and 1-year readmission for acute myocardial infarction in patients with AF compared with patients without AF. AF was associated with increased in-hospital mortality and an increased risk of death at 1-year follow-up. In patients who survived the STEMI episode, treatment with oral anticoagulants was associated with a lower risk of death at 1-year follow-up. This study shows a heavy prognostic impact of AF on HD patients who underwent STEMI.
心房颤动与接受血液透析合并ST段抬高型心肌梗死患者住院死亡率和1年死亡率增加相关:一项回顾性队列研究
基本原理及目的房颤(AF)在维持性血液透析(HD)患者和ST段抬高型心肌梗死(STEMI)患者中非常普遍。我们调查了房颤与入院STEMI的HD患者住院死亡率、1年死亡率和1年急性心肌梗死(AMI)再入院的关系。研究设计:基于大型管理数据库的回顾性队列研究。设置,2003年至2018年期间,138939例STEMI患者入院,其中1185例(8.5%)接受HD,从入院之日起随访至死亡、迁移或出院后1年。exposure stemi (International Classification of Diseases,第九次修订,Clinical Modification [ICD-9-CM] 410.x)作为主要出院诊断,维持性HD (ICD-9-CM 39.95;54.98;V560;V563.1;V563.2)和AF (ICD-9-CM 427.31)。院内全因死亡率(主要结局)、1年内全因死亡率和1年内AMI再入院(次要结局)。分析方法:多变量logistic回归和多变量Cox回归。结果1185例患者中有195例(16.5%)在入院时或住院期间发生房颤。在调整了可能的混杂因素后,房颤与窦性心律相关的住院死亡率更高(优势比[OR] = 1.57;95%可信区间[CI], 1.11-2.22)。房颤与较高的1年死亡率相关(危险比[HR] = 1.45;95% CI, 1.18-1.76),而与AMI的1年再入院率无关(HR = 1.05;95% ci, 0.72-1.53)。在存活出院的房颤患者中,只有不到20%的患者接受了口服抗凝治疗。在该亚组中,口服抗凝治疗与较低的1年死亡率相关(HR = 0.46;95% ci, 0.24-0.89)。局限性:由于不正确或不完整的编码、回顾性设计、出院后血栓栓塞事件的发生率以及未知的1年死亡率,可能存在偏倚。结论:在STEMI住院的HD患者中,saf非常普遍,并与不良的短期和长期预后相关。房颤(AF)在接受血液透析(HD)的肾衰竭患者和急性心肌梗死患者中都很常见。我们回顾性研究了房颤对1185例因ST段抬高型心肌梗死(STEMI)入院的HD患者的影响。我们比较了房颤患者与非房颤患者的住院死亡率、1年死亡率和1年急性心肌梗死再入院率。房颤与1年随访时住院死亡率增加和死亡风险增加相关。在STEMI事件存活的患者中,口服抗凝治疗与1年随访时较低的死亡风险相关。这项研究表明,房颤对STEMI患者的预后有重大影响。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


