Meniscal centralization significantly improve clinical outcomes and reduce meniscal extrusion with minimal complications: A systematic review
Abstract
Purpose
Meniscal extrusion alters joint biomechanics and accelerates cartilage degeneration, contributing to the progression of knee osteoarthritis (OA). Meniscal centralization techniques aim to reposition the meniscus, addressing extrusion and restoring load distribution. This systematic review aims to evaluate meniscal centralization's clinical and radiological outcomes, hypothesizing its efficacy in treating symptomatic meniscal extrusion with minimal complications.
Methods
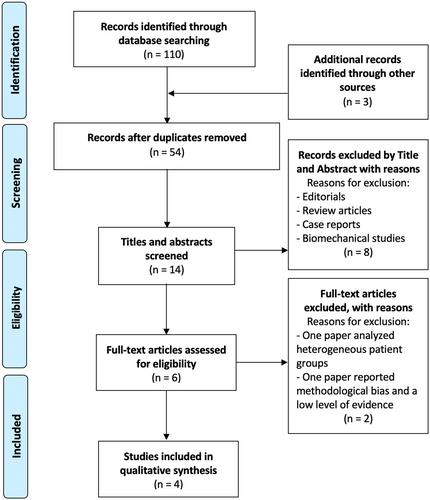
This review followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and was registered with PROSPERO (CRD42023484353). Literature searches were conducted in PubMed, Science Direct and Scopus. Studies reporting clinical and/or radiological outcomes of meniscal centralization with ≥24 months of follow-up were included. Data on demographics, surgical techniques, patient-reported outcome measures (PROMs), imaging findings and complications were extracted. Methodological quality was assessed using the ROBINS-I tool, and heterogeneity was evaluated via the I2 statistic.
Results
Four studies (113 patients, mean follow-up: 24–35 months) met inclusion criteria. Arthroscopic meniscal centralization with suture anchors significantly improved PROMs, including International Knee Documentation Committee (IKDC), Lysholm and Knee Injury and Osteoarthritis Outcome Score (KOOS) scores, demonstrating symptom relief and functional recovery. Lysholm scores improved from 46.0 to 96.5, KOOS pain from 47.4 to 88.9, and IKDC from 51.8 to 75.8 (p < 0.05 for all). Imaging showed reduced meniscal extrusion and improved joint space width. Complications were minimal, though one study reported a 26.9% failure rate due to incomplete healing and OA progression. Rehabilitation protocols allowed return to full activity within 4–6 months.
Conclusions
Meniscal centralization effectively reduces extrusion, improves clinical outcomes, and restores knee function with minimal complications. However, further long-term and comparative studies are needed to validate these findings and refine surgical indications.
Level of Evidence
Level IV.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


