An innovative self-stabilised 3D-printed artificial vertebral body designed for clinical application and comparison with the conventional implants
IF 5.9
1区 医学
Q1 ORTHOPEDICS
引用次数: 0
Abstract
Background
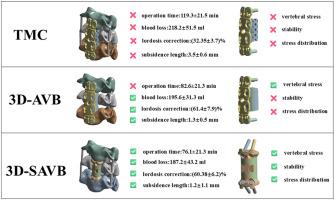
Corpectomy and bone defects reconstruction is a key surgical technique in spinal diseases treatment. Popular bone defect reconstruction methods include titanium mesh cage (TMC) fixation plate systems and traditional 3D-printed artificial vertebral body (3D-AVB). In our previous study, we conceptualised and created a self-stabilised 3D-printed artificial vertebral body (3D-SAVB) system and tested its clinical safety and efficacy, but have not compared with the conventional implants. This study was designed to compare our innovative 3D-SAVB system with a conventional 3D-AVB system, both mechanically and clinically.
Methods
This study included 33 patients with cervical spondylotic myelopathy who underwent single-level ACCF using the TMC, 3D-AVB, and 3D-SAVB systems. The operation time, intraoperative blood loss, neurological function recovery rate, average subsidence length, and cervical lordosis correction (C2-7 Cobb angle change) rates of the TMC, 3D-AVB, and 3D-SAVB groups were tested to compare their performance, and we selected four representative clinical cases with various diseases who underwent 3D-SAVB surgery for follow-up studies to demonstrate the clinical effect. In addition, finite element analysis was used to compare the stability, stress distribution, and artificial vertebral body stress of the 3D-SAVB, 3D-AVB, and TMC systems.
Results
The neurological function recovery rates of the TMC (84.8 ± 10.7 %), 3D-AVB (74.3 ± 7.9 %), and SAVB (85.99 ± 13.2 %) groups showed no significant difference (p > 0.05). The mean operation time of the TMC group (119.3 ± 21.5 min) is significant more than the 3D-SAVB (76.1 ± 23.1 mm) and 3D-AVB (82.6 ± 21.3 mm) groups (p < 0.05). The intraoperative blood loss of the TMC group (218.2 ± 51.5 ml) was significantly greater than that of the 3D-SAVB (187.6 ± 43.2 ml) and 3D-AVB groups (195.6 ± 31.3 ml) (p < 0.05). The mean subsidence length of the TMC group (3.5 ± 0.6 mm) was significantly greater than the 3D-AVB (1.3 ± 0.5 mm, p < 0.001) and 3D-SAVB (1.2 ± 1.1 mm, p = 0.002). The lordosis correction (C2-7 Cobb angle change) rate of the 3D-SAVB [(60.38 ± 6.2)%] and 3D-AVB [(61.4 ± 7.9)%] groups was significantly higher than that of the TMC group [(32.35 ± 3.7)%] (p < 0.05). Patients treated with the 3D-SAVB system achieved satisfactory treatment results with no postoperative complications during the follow-up period. The failed TMC fixation plate system underwent revision surgery using 3D-SAVB and demonstrated a superior prognosis. The biomechanical test showed that the 3D-SAVB system had greater longitudinal stability (p < 0.01), better stress distribution (p < 0.01), and less vertebral stress (p < 0.01) than the 3D-AVB and TMC systems.
Conclusion
These results demonstrate the mechanical advantages and great clinical application potential of our innovative 3D-SAVB system for challenging spinal surgeries.
Translational Potential of this Article
The 3D-SAVB system eliminates the need for supplementary fixation plates, reduces surgical complications like subsidence, and improves cervical lordosis correction. Its biomechanical superiority and clinical efficacy support its adoption as a next-generation spinal implant.
一种创新的自稳定3d打印人工椎体,专为临床应用而设计,并与传统植入物进行比较
背景椎体切除和骨缺损重建是脊柱疾病治疗的关键外科技术。常用的骨缺损重建方法包括钛网笼(TMC)固定钢板系统和传统的3d打印人工椎体(3D-AVB)。在我们之前的研究中,我们概念化并创建了一种自稳定的3d打印人工椎体(3D-SAVB)系统,并测试了其临床安全性和有效性,但尚未与传统植入物进行比较。本研究旨在比较我们创新的3D-SAVB系统与传统的3D-AVB系统在机械和临床方面的差异。方法本研究纳入33例脊髓型颈椎病患者,采用TMC、3D-AVB和3D-SAVB系统行单级ACCF。比较TMC组、3D-AVB组和3D-SAVB组的手术时间、术中出血量、神经功能恢复率、平均下陷长度、颈椎前凸矫正(C2-7 Cobb角变化)率,并选择4例具有代表性的临床病例行3D-SAVB手术进行随访研究,以证明其临床效果。此外,采用有限元分析比较3D-SAVB、3D-AVB和TMC系统的稳定性、应力分布和人工椎体应力。结果TMC组(84.8±10.7%)、3D-AVB组(74.3±7.9%)、SAVB组(85.99±13.2%)的神经功能恢复率差异无统计学意义(p >;0.05)。TMC组平均手术时间(119.3±21.5 min)显著高于3D-SAVB组(76.1±23.1 mm)和3D-AVB组(82.6±21.3 mm) (p <;0.05)。TMC组术中出血量(218.2±51.5 ml)明显大于3D-SAVB组(187.6±43.2 ml)和3D-AVB组(195.6±31.3 ml) (p <;0.05)。TMC组的平均下陷长度(3.5±0.6 mm)显著大于3D-AVB组(1.3±0.5 mm), p <;0.001)和3D-SAVB(1.2±1.1 mm, p = 0.002)。3D-SAVB组前凸矫正(C2-7 Cobb角改变)率[(60.38±6.2)%]和3D-AVB组[(61.4±7.9)%]显著高于TMC组[(32.35±3.7)%](p <;0.05)。3D-SAVB系统治疗的患者在随访期间均取得满意的治疗效果,无术后并发症发生。失败的TMC固定钢板系统采用3D-SAVB进行翻修手术,预后良好。生物力学试验表明,3D-SAVB系统具有更大的纵向稳定性(p <;0.01),应力分布较好(p <;0.01),椎体应力较小(p <;0.01),高于3D-AVB和TMC系统。结论本发明的3D-SAVB系统在具有挑战性的脊柱手术中具有机械优势和巨大的临床应用潜力。3D-SAVB系统消除了对辅助固定钢板的需要,减少了手术并发症,如下沉,并改善了颈椎前凸矫正。其生物力学优势和临床疗效支持其作为下一代脊柱植入物的采用。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Journal of Orthopaedic Translation
Medicine-Orthopedics and Sports Medicine
CiteScore
11.80
自引率
13.60%
发文量
91
审稿时长
29 days
期刊介绍:
The Journal of Orthopaedic Translation (JOT) is the official peer-reviewed, open access journal of the Chinese Speaking Orthopaedic Society (CSOS) and the International Chinese Musculoskeletal Research Society (ICMRS). It is published quarterly, in January, April, July and October, by Elsevier.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


