Exploring longitudinal physiologic stress measurement and sleep quality interventions to improve psychological well-being in nurses: a pilot study.
IF 2.2
Q2 PSYCHOLOGY, CLINICAL
Allison A Norful, Krystyna de Jacq, Jiawen Zhao, Yuandi Gao, Kathryn Asadoorian, Yilei Yang, Hyun Jin Jung, Ari Shechter
下载PDF
{"title":"Exploring longitudinal physiologic stress measurement and sleep quality interventions to improve psychological well-being in nurses: a pilot study.","authors":"Allison A Norful, Krystyna de Jacq, Jiawen Zhao, Yuandi Gao, Kathryn Asadoorian, Yilei Yang, Hyun Jin Jung, Ari Shechter","doi":"10.1080/21642850.2025.2503376","DOIUrl":null,"url":null,"abstract":"<p><strong>Introduction: </strong>Rates of depression, burnout, and anxiety among nurses are high. Improving sleep quality may mitigate psychological distress, but research on effective sleep interventions for nurses is limited. This pilot study explored the preliminary effects of the Somni© sleep quality kit on sleep, stress, and psychological health among nurses using continuous physiologic data from the Oura ring©.</p><p><strong>Methods: </strong>A prospective pilot trial was conducted with 25 nurses. Participants wore the Oura ring© for eight weeks to collect data on heart rate variability (HRV) and sleep. The Somni© sleep kit, containing evidence-based sleep aids, was introduced from weeks 4-8. Participants completed surveys at baseline, 4, and 8 weeks to assess sleep quality, stress, burnout, and depressive symptoms. Data were analyzed using paired t-tests and linear mixed-effect models.</p><p><strong>Results: </strong>The sample was predominantly White (64%), non-Hispanic (88%), and female (84%). Lavender spray and white noise machines were the most frequently used sleep aids. Self-reported sleep latency significantly decreased (<i>p</i> = 0.03), with a trend toward improved sleep quality. No significant changes were observed in physiologic metrics or depressive symptoms. Effect sizes ranged from moderate to small, with the greatest improvement in sleep latency.</p><p><strong>Discussion: </strong>The Somni© sleep kit showed potential for improving self-reported sleep quality and sleep latency, especially through non-pharmacologic interventions. While the results were mixed, this study supports the feasibility of using wearable devices to track sleep and stress in nurses. Future research should include larger samples and investigate the long-term effects of sleep interventions on nurses' mental health.</p>","PeriodicalId":12891,"journal":{"name":"Health Psychology and Behavioral Medicine","volume":"13 1","pages":"2503376"},"PeriodicalIF":2.2000,"publicationDate":"2025-05-13","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12077477/pdf/","citationCount":"0","resultStr":null,"platform":"Semanticscholar","paperid":null,"PeriodicalName":"Health Psychology and Behavioral Medicine","FirstCategoryId":"1085","ListUrlMain":"https://doi.org/10.1080/21642850.2025.2503376","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"2025/1/1 0:00:00","PubModel":"eCollection","JCR":"Q2","JCRName":"PSYCHOLOGY, CLINICAL","Score":null,"Total":0}
引用次数: 0
引用
批量引用
Abstract
Introduction: Rates of depression, burnout, and anxiety among nurses are high. Improving sleep quality may mitigate psychological distress, but research on effective sleep interventions for nurses is limited. This pilot study explored the preliminary effects of the Somni© sleep quality kit on sleep, stress, and psychological health among nurses using continuous physiologic data from the Oura ring©.
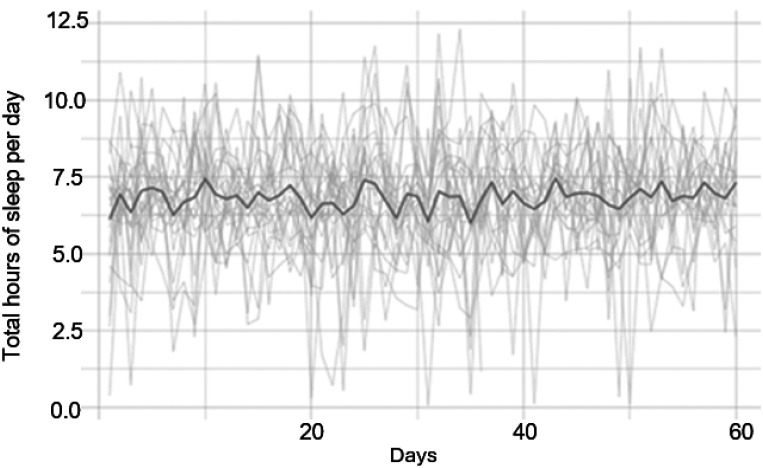
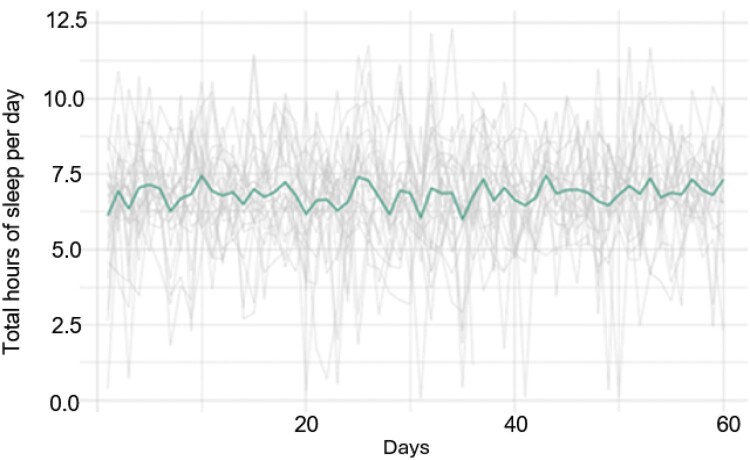
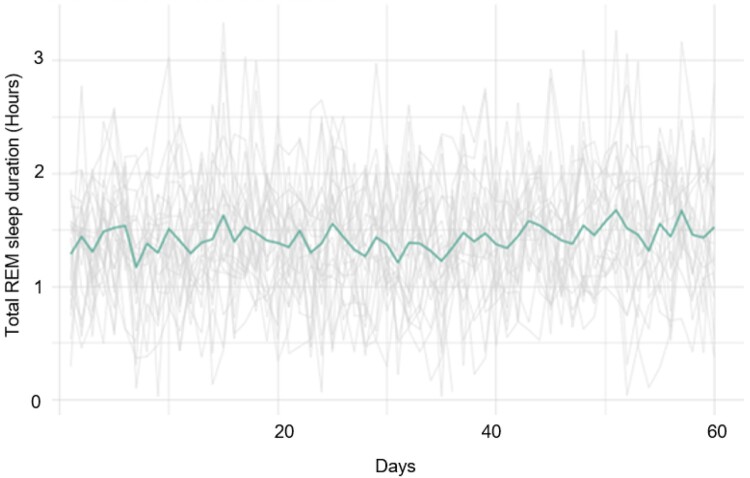
Methods: A prospective pilot trial was conducted with 25 nurses. Participants wore the Oura ring© for eight weeks to collect data on heart rate variability (HRV) and sleep. The Somni© sleep kit, containing evidence-based sleep aids, was introduced from weeks 4-8. Participants completed surveys at baseline, 4, and 8 weeks to assess sleep quality, stress, burnout, and depressive symptoms. Data were analyzed using paired t-tests and linear mixed-effect models.
Results: The sample was predominantly White (64%), non-Hispanic (88%), and female (84%). Lavender spray and white noise machines were the most frequently used sleep aids. Self-reported sleep latency significantly decreased (p = 0.03), with a trend toward improved sleep quality. No significant changes were observed in physiologic metrics or depressive symptoms. Effect sizes ranged from moderate to small, with the greatest improvement in sleep latency.
Discussion: The Somni© sleep kit showed potential for improving self-reported sleep quality and sleep latency, especially through non-pharmacologic interventions. While the results were mixed, this study supports the feasibility of using wearable devices to track sleep and stress in nurses. Future research should include larger samples and investigate the long-term effects of sleep interventions on nurses' mental health.
探索纵向生理应激测量和睡眠质量干预以改善护士的心理健康:一项试点研究。
护士中抑郁、倦怠和焦虑的比例很高。改善睡眠质量可以减轻护士的心理困扰,但对护士有效睡眠干预的研究有限。本初步研究利用来自Oura环©的连续生理数据,探讨了Somni©睡眠质量套件对护士睡眠、压力和心理健康的初步影响。方法:对25名护士进行前瞻性先导试验。参与者佩戴Oura戒指©八周,以收集心率变异性(HRV)和睡眠数据。从第4-8周开始使用含有循证睡眠辅助工具的Somni©睡眠工具包。参与者在基线、4周和8周完成调查,以评估睡眠质量、压力、倦怠和抑郁症状。数据分析采用配对t检验和线性混合效应模型。结果:样本以白人(64%)、非西班牙裔(88%)和女性(84%)为主。薰衣草喷雾和白噪音机是最常用的助眠剂。自我报告的睡眠潜伏期显著降低(p = 0.03),睡眠质量有改善的趋势。在生理指标或抑郁症状方面未观察到显著变化。效应大小从中等到小不等,睡眠潜伏期的改善最大。讨论:Somni©睡眠套件显示出改善自我报告的睡眠质量和睡眠潜伏期的潜力,特别是通过非药物干预。虽然结果好坏参半,但这项研究支持了使用可穿戴设备跟踪护士睡眠和压力的可行性。未来的研究应该包括更大的样本,并调查睡眠干预对护士心理健康的长期影响。
本文章由计算机程序翻译,如有差异,请以英文原文为准。

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


