The formal EU-US Meniscus Rehabilitation 2024 Consensus: An ESSKA-AOSSM-AASPT initiative. Part I—Rehabilitation management after meniscus surgery (meniscectomy, repair and reconstruction)
Abstract
Purpose
The aim of part one of this EU-US consensus was to combine literature research and expertise to provide recommendations for the usage of rehabilitation (including physical therapy) of patients undergoing surgical treatment for degenerative meniscus lesions or acute meniscus tears (including meniscectomy, repair, or reconstruction). Prevention programmes, non-operative treatment of acute tears and degenerative lesions, return to sports and patient-reported outcome measures will be presented in a part II article.
Methods
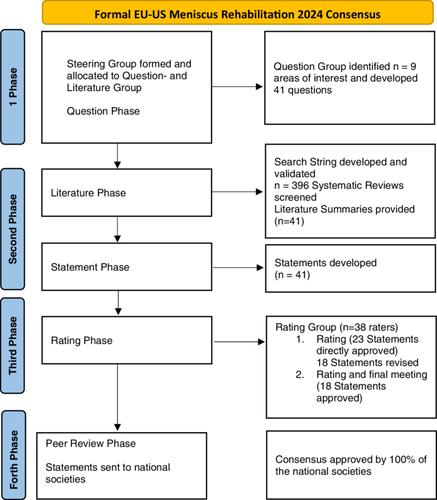
This consensus followed the European Society for Sports Traumatology and Arthroscopy (ESSKA)'s ‘formal consensus’ methodology. For this combined ESSKA, American Orthopedic Society for Sports Medicine and American Academy of Sports Physical Therapy initiative, 67 experts (26 in the steering group and 41 in the rating group) from 14 countries (US and 13 European countries), including orthopaedic surgeons, sports medicine doctors and physiotherapists were involved. Steering group members established guiding questions, searched the literature and proposed statements. Rating group members assessed the statements according to a Likert scale and provided grades of recommendations, reaching a final agreement about rehabilitation of the knee after meniscus surgery. Final documents were then assessed by a peer review group to address the geographical adaptability.
Results
The overall level of evidence in the literature was low. Of the 19 questions (leading to 29 statements), 1 received a Grade A of recommendation, 2 a Grade B, 9 a Grade C and 17 a Grade D. Nevertheless, the mean median rating of all questions was 8.2/9 (9 being the highest rating on a scale of 1–9). The global mean rating was 8.4 ± 0.2, indicating a high agreement. Rehabilitation depends on the type of lesion, the treatment performed and is the same after medial or lateral meniscus surgery. Rehabilitation after meniscectomy should follow a criterion-based rehabilitation protocol, based on milestones rather than a time-based protocol. After meniscus repair and reconstruction, rehabilitation should be progressed according to both time and criterion-based milestones.
Conclusion
Rehabilitation after meniscus surgery is a debated topic that may influence surgical outcomes if not optimally performed. This international formal consensus established clear, updated and structured recommendations for both surgeons and physiotherapists treating patients after meniscus surgery.
Level of Evidence
Level I, consensus.



 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


