Valve-sparing aortic root replacement in bicuspid aortic valves—the reimplantation technique: A multicenter study
IF 4.4
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Thoracic and Cardiovascular Surgery
Pub Date : 2025-10-01
DOI:10.1016/j.jtcvs.2025.02.008
引用次数: 0
Abstract
Objective
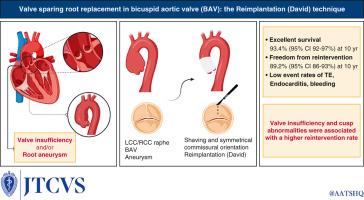
Reported outcomes in patients with bicuspid aortic valves (BAVs) undergoing valve-sparing aortic root replacement (VSRR) are scarce. This study aims to evaluate outcomes in patients with BAV using the reimplantation (David) technique.
Methods
Consecutive adult patients with BAV, aortic root aneurysm, and/or aortic valve insufficiency (AI) undergoing VSRR (reimplantation) were included from 5 centers experienced in reimplantation procedures. Patients were subcategorized into 2 groups with different primary indications for operation: (1) aneurysm, and (2) isolated AI. Exclusion criteria included acute aortic dissection, endocarditis, and valvular-stenosis.
Results
In total, 498 patients were included. Mean age was 45.4 years (±11.8 years); median follow-up was 5.4 years (interquartile range, 2.3-8.7 years). Group 1 included aneurysm (n = 144) and group 2 included AI (n = 354). There was 1 in-hospital death. Survival (overall) was 93.4% (95% confidence interval [CI], 92-97%) at 10 years, with no difference between groups (P = .93) observed. Freedom from reintervention at 1 year was 99.1% (95% CI, 99%-100%), at 5 years 95.4% (95% CI, 93%-97%), and at 10 years 89.2% (95% CI, 86%-93%) for patients with aneurysm 100% at 1 year and 95.4% (95% CI, 92%-98%) at 10 years; and for AI 98.9% (95% CI, 98%-99%) at 1 year and 86.4% (95% CI, 83%-91%) at 10 years. Cusp fenestrations (P = .01), prolapse (P = .04), and isolated AI (0.03) were associated with greater hazard of reintervention.
Conclusions
This multicenter study shows excellent results after VSRR reimplantation procedure in patients with BAV and aortic aneurysm and/or valve insufficiency. Isolated AI and cusp abnormalities are associated with greater reintervention rates and may reflect more advanced leaflet disease. The reimplantation technique, when performed in expert centers, appears to be an excellent treatment strategy in BAV.
二尖瓣主动脉瓣保留主动脉根部置换术:一项多中心研究。
目的:报道双尖瓣主动脉瓣(BAV)患者行保留瓣膜根置换术(VSRR)的结果很少。本研究旨在评估BAV患者使用David技术的预后。方法:连续纳入来自5个中心的BAV、主动脉根部动脉瘤和/或瓣膜功能不全(AI)的成人患者,进行VSRR(再植入术)。根据不同的主要手术指征将患者分为两组:1)动脉瘤组和2)孤立性AI组。排除标准:急性主动脉夹层、心内膜炎、瓣膜狭窄。结果:纳入498例患者。平均年龄45.4(±11.8)岁;中位随访时间为5.4年(IQR为2.3-8.7年)。1组:动脉瘤(N=144), 2组:AI (N=354)。有一人在医院死亡10年生存率(总体)为93.4% (95% CI 92-97%),组间无差异(p=0.93)。1年无再干预率为99.1% (95% CI 99-100%), 5年为95.4% (95% CI 93-97%), 10年为89.2% (95% CI 86-93%);动脉瘤患者1年为100%,10年为95.4% (95% CI 92-98%);AI 1年为98.9% (95% CI 98-99%), 10年为86.4% (95% CI 83-91%)。尖峰开孔(P=0.01)、脱垂(P=0.04)和孤立的AI(0.03)与再干预风险较高相关。结论:这项多中心研究显示,BAV合并主动脉瘤和/或瓣膜功能不全的患者行VSRR、再植手术后效果良好。孤立的AI和尖端异常与较高的再干预率相关,可能反映更晚期的小叶疾病。在专家中心进行的再植技术似乎是BAV的一种极好的治疗策略。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
11.20
自引率
10.00%
发文量
1079
审稿时长
68 days
期刊介绍:
The Journal of Thoracic and Cardiovascular Surgery presents original, peer-reviewed articles on diseases of the heart, great vessels, lungs and thorax with emphasis on surgical interventions. An official publication of The American Association for Thoracic Surgery and The Western Thoracic Surgical Association, the Journal focuses on techniques and developments in acquired cardiac surgery, congenital cardiac repair, thoracic procedures, heart and lung transplantation, mechanical circulatory support and other procedures.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


