Donor selection in T-cell-replete haploidentical donor peripheral blood stem cell transplantation
IF 12.8
1区 医学
Q1 HEMATOLOGY
引用次数: 0
Abstract
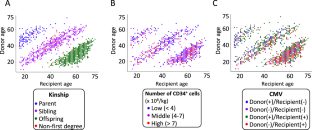
The effects of donor characteristics on outcomes after T-cell-replete (TCR) haploidentical donor peripheral blood stem cell transplantation (PBSCT) with post-transplant cyclophosphamide (PTCy) or low-dose antithymocyte globulin (ATG) remain unclear. We evaluated the impact in 1,677 patients who received a PTCy protocol (PTCy-haplo; n = 1,107) or low-dose ATG protocol (ATG-haplo; n = 570). A low CD34+ cell dose (<4 ×106/kg) was the only donor characteristic associated with worse overall survival (OS) after PTCy-haplo (adjusted hazard ratios [aHR] = 1.49, P = 0.008), whereas increasing donor age by decade (aHR = 1.12, P = 0.008) and human leukocyte antigen 2-3 antigen mismatches (aHR = 1.46, P = 0.010), compared to HLA 0-1 antigen mismatches, were associated with worse OS after ATG-haplo. Increasing donor age was associated with a high risk of grade III–IV acute GVHD both after PTCy-haplo (HR: 1.32, P = 0.009) and ATG-haplo (HR: 1.22, P = 0.006). Offspring donors had better relapse-free survival and GVHD-free relapse-free survival than sibling donors after ATG-haplo. Our data highlights the donor characteristics associated with improved transplant outcomes after TCR haploidentical donor PBSCT with PTCy or low-dose ATG.

t细胞单倍体外周血干细胞移植的供体选择
供体特征对移植后使用环磷酰胺(PTCy)或低剂量抗胸腺细胞球蛋白(ATG)进行t细胞填充(TCR)单倍体供体外周血干细胞移植(PBSCT)后预后的影响尚不清楚。我们评估了1,677名接受PTCy方案的患者的影响(PTCy-haplo;n = 1107)或低剂量ATG方案(ATG-haplo;n = 570)。低CD34+细胞剂量(<4 ×106/kg)是唯一与PTCy-haplo后总生存率(OS)较差相关的供体特征(校正风险比[aHR] = 1.49, P = 0.008),而与HLA 0-1抗原错配相比,供体年龄增加10岁(aHR = 1.12, P = 0.008)和人白细胞抗原2-3抗原错配(aHR = 1.46, P = 0.010)与ATG-haplo后OS较差相关。供者年龄的增加与PTCy-haplo (HR: 1.32, P = 0.009)和ATG-haplo (HR: 1.22, P = 0.006)后III-IV级急性GVHD的高风险相关。ATG-haplo后,后代供者的无复发生存率和gvhd无复发生存率优于兄弟姐妹供者。我们的数据强调了在TCR单倍体相同供体PBSCT加PTCy或低剂量ATG后,供体特征与移植结果的改善相关。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Leukemia
医学-血液学
CiteScore
18.10
自引率
3.50%
发文量
270
审稿时长
3-6 weeks
期刊介绍:
Title: Leukemia
Journal Overview:
Publishes high-quality, peer-reviewed research
Covers all aspects of research and treatment of leukemia and allied diseases
Includes studies of normal hemopoiesis due to comparative relevance
Topics of Interest:
Oncogenes
Growth factors
Stem cells
Leukemia genomics
Cell cycle
Signal transduction
Molecular targets for therapy
And more
Content Types:
Original research articles
Reviews
Letters
Correspondence
Comments elaborating on significant advances and covering topical issues
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


