Efficacy and hypoglycaemia outcomes with once-weekly insulin icodec versus once-daily basal insulin in individuals with type 2 diabetes by kidney function: A post hoc participant-level analysis of the ONWARDS 1–5 trials
Abstract
Aim
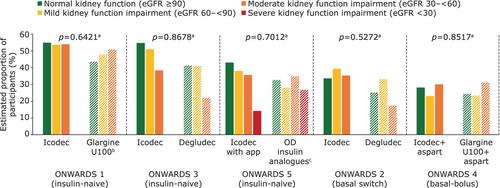
This post hoc analysis of ONWARDS 1–5 assessed the efficacy and hypoglycaemia outcomes with once-weekly insulin icodec (icodec) versus once-daily basal insulin comparators (degludec, glargine U100 or glargine U300) in insulin-naive (ONWARDS 1, 3 and 5) and insulin-experienced (ONWARDS 2 and 4) adults (aged ≥18 years) with type 2 diabetes (T2D) by kidney function subgroup.
Materials and Methods
Treatment outcomes were analysed by trial according to kidney function subgroup (estimated glomerular filtration rate [eGFR] ≥90; eGFR 60–<90; eGFR 30–<60; eGFR <30; all mL/min/1.73m2). Severe kidney function impairment (eGFR <30) at screening was an exclusion criterion for ONWARDS 1–4, but not ONWARDS 5.
Results
ONWARDS 1–5 included 3765 participants; 3763 were included in this analysis. In ONWARDS 1, 3 and 5, there were no statistically significant treatment interactions by kidney function subgroup for change in glycated haemoglobin (HbA1c) from baseline to end of treatment (EOT); there were statistically significant subgroup interactions in ONWARDS 2 and 4 (both p-interaction <0.05). Change in body weight (baseline to EOT) across kidney function subgroups was comparable between treatment arms. Across trials, there was no consistent trend by kidney function subgroup for mean weekly insulin dose during the last 2 weeks of treatment or rates of combined clinically significant or severe hypoglycaemia. There were no statistically significant treatment interactions by kidney function subgroup for the achievement of HbA1c <7% without clinically significant or severe hypoglycaemia; all p-interaction >0.05.
Conclusions
Efficacy and hypoglycaemia outcomes of icodec versus once-daily comparators were generally consistent among adults with T2D, regardless of kidney function.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


