Use of a Nutritional Risk Assessment Tool to Guide Early Enteral Nutrition among Mechanically Ventilated Trauma Patients
引用次数: 0
Abstract
Background
The Modified Nutritional Risk in Critically Ill (mNUTRIC) score has been proposed as a tool to identify hospitalized patients at risk for malnutrition who may benefit from early enteral nutrition (EN) therapy.
Objective
Our goal was to determine if mNUTRIC scores could predict, at time of intensive care unit admission, which mechanically ventilated trauma patients were at risk for malnutrition and might benefit from early EN, as indicated by reduced mortality.
Methods
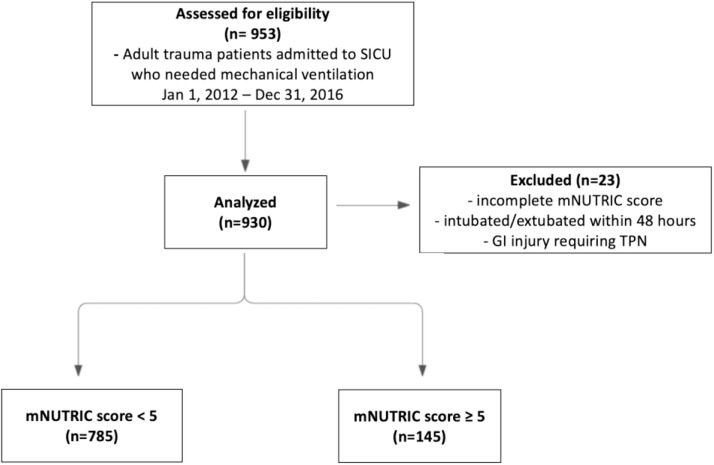
We conducted a retrospective chart review of all adult trauma patients requiring mechanical ventilation for at least 48 hours between 01/21/2012 and 12/31/2016, reviewing inpatient medical records, demographic data, disease markers, injury severity, and comorbidities. Bivariate statistics and multivariate regression analyses were used to investigate the correlation between time of EN initiation and mortality rates, as well as the relationship of mNUTRIC scores with EN commencement with early EN initiation being ≤48 hours and malnutrition risk mNUTRIC ≥5.
Results
Among 931 patients reviewed, bivariate analysis showed higher mNUTRIC scores correlated with older, sicker patients and higher mortality. However, multivariate analysis revealed no significant association between higher mNUTRIC scores and increased mortality (OR 1.2, 95% CI 0.7-2.1, p=0.52). Although most patients received EN within 48 hours, there was no association between mNUTRIC score and timing of EN initiation after adjusting for demographic variables and illness severity.
Conclusions
Our findings indicate that while the mNUTRIC score can effectively identify malnutrition risk, it does not meaningfully inform early EN initiation timing nor predict mortality in mechanically ventilated trauma patients.
使用营养风险评估工具指导机械通气创伤患者早期肠内营养。
背景:危重症患者改良营养风险(mNUTRIC)评分已被提出作为一种工具来识别有营养不良风险的住院患者,这些患者可能受益于早期肠内营养(EN)治疗。目的:我们的目的是确定在重症监护病房入院时,mNUTRIC评分是否可以预测机械通气创伤患者是否有营养不良的风险,并可能从早期EN中获益,这表明死亡率降低。方法:回顾性分析2012年1月21日至2016年12月31日期间所有需要机械通气至少48小时的成人创伤患者,回顾住院病历、人口统计资料、疾病标志物、损伤严重程度和合并症。采用双变量统计和多变量回归分析,探讨EN起始时间与死亡率的相关性,以及EN起始时间≤48小时、营养不良风险mNUTRIC≥5分与EN起始时间的关系。结果:在931例患者中,双变量分析显示,较高的mNUTRIC评分与年龄较大、病情较重的患者和较高的死亡率相关。然而,多变量分析显示较高的mNUTRIC评分与死亡率增加之间没有显著关联(OR 1.2, 95% CI 0.7-2.1, p=0.52)。虽然大多数患者在48小时内接受了EN,但在调整人口统计学变量和疾病严重程度后,mNUTRIC评分与EN开始时间之间没有关联。结论:我们的研究结果表明,尽管mNUTRIC评分可以有效地识别营养不良风险,但它并不能为机械通气创伤患者的早期EN起始时间提供有意义的信息,也不能预测死亡率。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

American journal of medicine open
Medicine and Dentistry (General)
自引率
0.00%
发文量
0
审稿时长
47 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


