Surgery for Patients With cT3/4N2M0, Stage IIIB NSCLC. Is It Time to Redefine Resectability?
IF 3.5
Q2 ONCOLOGY
引用次数: 0
Abstract
Introduction
Chemoradiation followed by durvalumab is considered a standard approach for patients with locally advanced NSCLC. With improvements in perioperative and neoadjuvant approaches, there is renewed interest in offering surgery to carefully selected patients with cT3/4N2 stage IIIB cancer. We sought to assess survival outcomes after surgery as part of a multimodality treatment regimen for these patients.
Methods
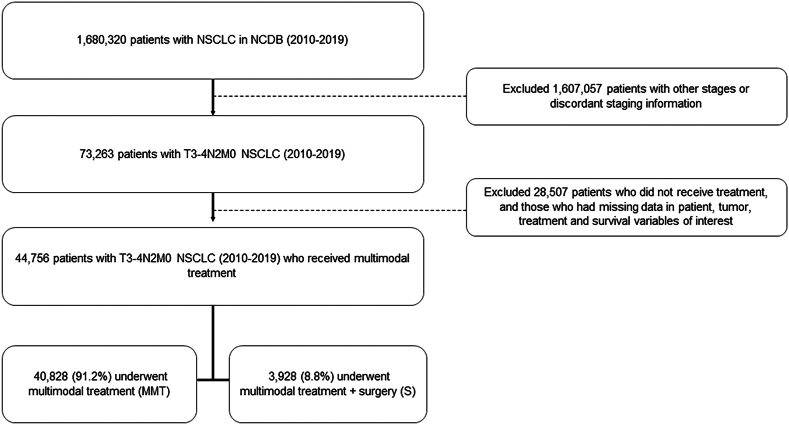
Patients with cT3/T4N2M0 NSCLC who received surgery (S) as part of a multimodality approach and patients receiving multimodality treatment without surgery (chemoradiation [CRT] or systemic therapy only) were identified in the National Cancer Database (2010–2019). We evaluated factors associated with the receipt of S (logistic regression). After propensity matching, we estimated the overall survival (OS) of patients who received S and compared with those who received CRT (Kaplan-Meier and Cox regression).
Results
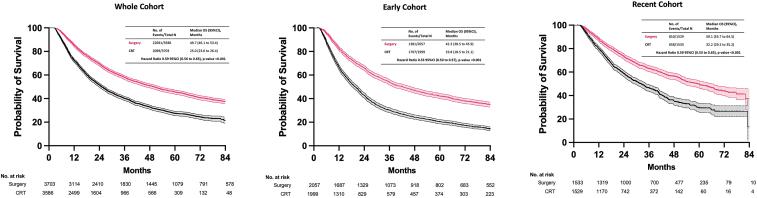
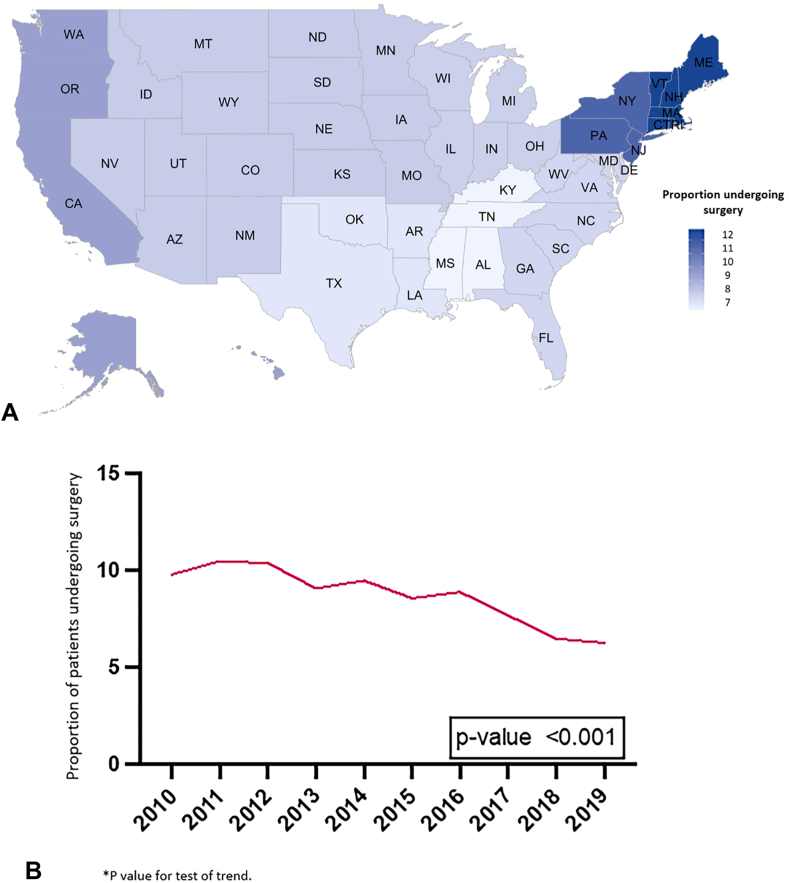
A total of 44,756 patients were identified, of whom 3928 (8.8%) underwent S, 29,798 (66.6%) CRT, and 11,030 (24.6%) systemic therapy only. Fewer comorbidities (Charlson-Deyo index 0 or 1, adjusted OR [aOR]: 1.22, 95% confidence interval [CI]: 1.05–1.42), treatment at an academic facility (aOR: 1.70, 95% CI: 1.52–1.89), private insurance (aOR: 2.44, 95% CI: 1.61–3.69), adenocarcinoma histology (aOR: 1.48, 95% CI: 1.22–1.79), and clinical T3 stage (<7 cm, aOR: 1.70, 95% CI: 1.53–1.89) were associated with S. In well-balanced, propensity-matched cohorts, patients selected for S had better OS compared with those who underwent CRT (hazard ratio 0.59, 95% CI: 0.56–0.63, p < 0.001) (median OS 49.7 versus 25.0 mo).
Conclusions
In this retrospective cohort analysis, patients with cT3/4N2, stage IIIB NSCLC who underwent surgical resection had better OS compared with those patients treated with CRT. Careful patient selection is undoubtedly critical, but stage IIIB designation alone should not exclude patients from surgical consideration.
cT3/4N2M0 iii期非小细胞肺癌的手术治疗是时候重新定义可切除性了吗?
化疗后的durvalumab被认为是局部晚期NSCLC患者的标准方法。随着围手术期和新辅助方法的改进,对精心挑选的cT3/4N2期IIIB癌症患者进行手术治疗的兴趣重新燃起。我们试图评估这些患者手术后的生存结果,作为多模式治疗方案的一部分。方法:在国家癌症数据库(2010-2019)中确定了接受手术(S)作为多模式方法一部分的cT3/T4N2M0 NSCLC患者和接受多模式非手术治疗(放化疗[CRT]或仅全身治疗)的患者。我们评估了与接收S相关的因素(逻辑回归)。倾向匹配后,我们估计了接受S治疗的患者的总生存率(OS),并与接受CRT治疗的患者进行了比较(Kaplan-Meier和Cox回归)。结果:共确定44,756例患者,其中3928例(8.8%)接受S, 29,798例(66.6%)接受CRT, 11,030例(24.6%)接受全身治疗。合共病较少(Charlson-Deyo指数0或1,校正or [aOR]: 1.22, 95%可信区间[CI]: 1.05-1.42),在学术机构接受治疗(aOR: 1.70, 95% CI: 1.52-1.89),私人保险(aOR: 2.44, 95% CI: 1.61-3.69),腺癌组织学(aOR: 1.48, 95% CI: 1.22-1.79),临床T3分期(p < 0.001)(中位OS 49.7 vs 25.0个月)。结论:在这项回顾性队列分析中,cT3/4N2, IIIB期NSCLC患者接受手术切除的OS比接受CRT治疗的患者更好。谨慎的患者选择无疑是至关重要的,但仅为IIIB期不应排除患者的手术考虑。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

JTO Clinical and Research Reports
Medicine-Oncology
CiteScore
4.20
自引率
0.00%
发文量
145
审稿时长
19 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


