Oncological outcomes after radical prostatectomy of localized prostate cancer: stratified by magnetic resonance imaging and risk classification
IF 2.6
2区 医学
Q2 UROLOGY & NEPHROLOGY
引用次数: 0
Abstract
Background
We investigated whether combining T2-weighted magnetic resonance imaging (MRI) findings and clinical risk categories improves upon established prognostic indicators of oncological outcomes in prostate cancer.
Methods
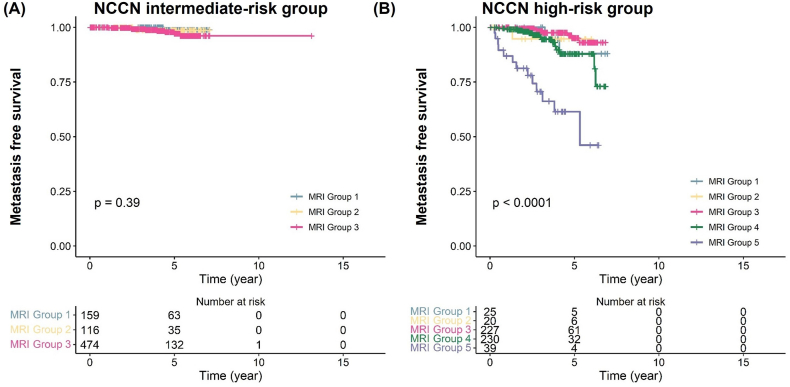
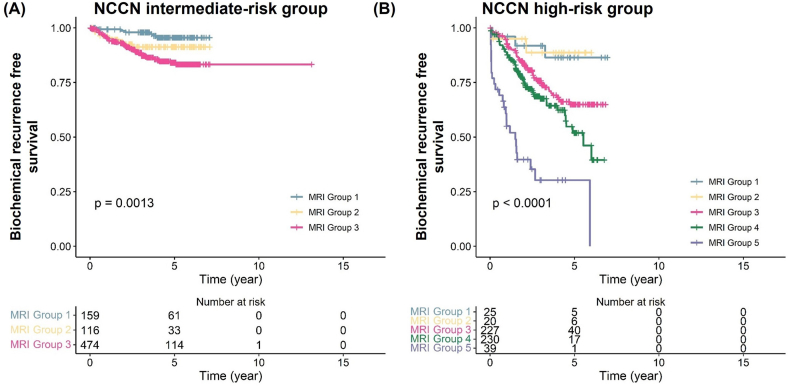
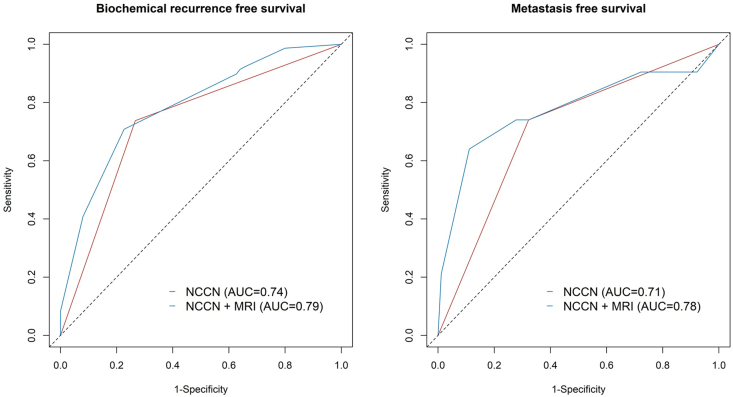
Patients who underwent radical prostatectomy, but not preoperative hormone therapy, radiotherapy, or chemotherapy, for localized prostate cancer at Seoul National University Bundang Hospital from October 2007 to April 2016 were included. MRIs were classified according to the Prostate Imaging-Reporting and Data System (PI-RADS). Patients were divided into the following five groups: 1, no focal suspicious lesion; 2, organ-confined suspicious lesion PI-RADS ≤3; 3, organ-confined suspicious lesion PI-RADS 4 or 5; 4, suspicious lesion with extraprostatic extension (EPE), no seminal vesicle invasion (SVI); 5, suspicious lesion with EPE and SVI. Risk classified according to the National Comprehensive Cancer Network (NCCN) and MRI findings were combined to analyze survival curves for biochemical recurrence (BCR)-free and metastasis-free survival. The area under a time-dependent receiver operating characteristic was analyzed for event prediction after 5 years.
Results
We analyzed 1,290 patients. In multivariate Cox regression models, PI-RADS ≥4 (hazard ratio [HR] 2.33, P < 0.001), EPE (HR 1.46, P = 0.027), SVI (HR 5.03, P < 0.001) and NCCN high-risk (HR 2.33, 95% CI 1.66-3.26, P < 0.001) were associated with BCR. For metastasis, EPE (HR 2.33, P = 0.047), SVI (HR 13.08, P < 0.001) and NCCN high-risk (HR 2.78, P = 0.026) were independent risk factors. Depending on MRI group, BCR-free survival significantly decreased in NCCN intermediate-risk (P = 0.001) and high-risk (P < 0.001) groups, and metastasis-free survival decreased in the intermediate-risk group (P = 0.39) and significantly decreased in the high-risk (P < 0.001) group. Adding MRI group to NCCN risk classification significantly improved the predictive accuracy for BCR in comparison with NCCN risk classification alone (P = 0.042), but not for metastasis (P = 0.012).
Conclusion
Combining prostate MRI with NCCN risk classification improves the prediction value of BCR following radical prostatectomy for localized prostate cancer.
局部前列腺癌根治性前列腺切除术后的肿瘤预后:磁共振成像分层和风险分类。
背景:我们研究了t2加权磁共振成像(MRI)结果和临床风险分类是否能改善前列腺癌肿瘤预后的既定预后指标。方法:纳入2007年10月至2016年4月在首尔国立大学盆唐医院接受根治性前列腺切除术,但术前未接受激素治疗、放疗或化疗的局限性前列腺癌患者。根据前列腺成像报告和数据系统(PI-RADS)对mri进行分类。患者分为以下5组:1、无局灶性可疑病变;2、器官局限性可疑病变PI-RADS≤3;3、器官局限性可疑病变PI-RADS为4或5;4、可疑病变伴前列腺外展(EPE),无精囊侵犯(SVI);5、可疑病灶伴EPE、SVI。根据国家综合癌症网络(NCCN)和MRI结果进行风险分类,分析无生化复发(BCR)和无转移生存的生存曲线。分析了时变接收机工作特征下的5年后事件预测面积。结果:我们分析了1290例患者。在多因素Cox回归模型中,PI-RADS≥4(危险比[HR] 2.33, P P = 0.027)、SVI (HR 5.03, P P = 0.047)、SVI (HR 13.08, P P = 0.026)为独立危险因素。不同MRI组,NCCN中危(P = 0.001)和高危(P = 0.39)患者无bcr生存率显著降低,高危(P = 0.042)患者无bcr生存率显著降低,而转移患者无bcr生存率显著降低(P = 0.012)。结论:前列腺MRI结合NCCN风险分级提高了前列腺根治术后BCR对局限性前列腺癌的预测价值。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Prostate International
Medicine-Urology
CiteScore
4.40
自引率
26.70%
发文量
40
审稿时长
35 days
期刊介绍:
Prostate International (Prostate Int, PI), the official English-language journal of Asian Pacific Prostate Society (APPS), is an international peer-reviewed academic journal dedicated to basic and clinical studies on prostate cancer, benign prostatic hyperplasia, prostatitis, and ...
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


