Ectopic pancreatic tissue in the gallbladder: A rare incidental finding in a cholecystectomy specimen – A case report
IF 0.7
Q4 SURGERY
引用次数: 0
Abstract
Introduction
Ectopic pancreatic tissue (EPT) is a rare congenital anomaly characterized by the presence of pancreatic tissue in an abnormal location, separate from the pancreas, without any anatomical or vascular connection to it. This anomaly is often an incidental finding during operation or autopsy. This peculiarity poses clinical and radiological challenges for surgeons, particularly during laparoscopic or open procedures.
Case report
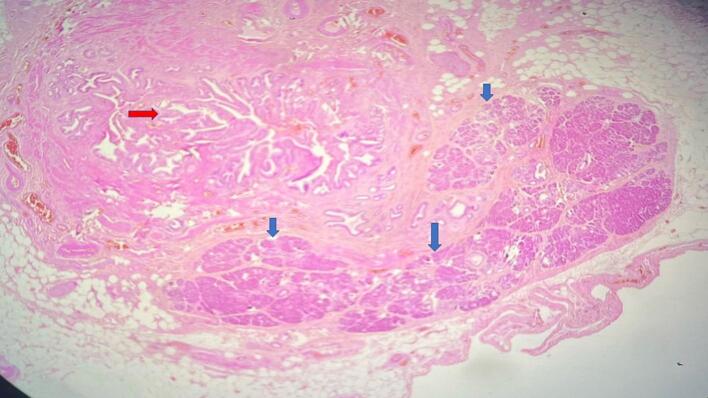
This article presents a compelling case of EPT, discovered incidentally during a planned laparoscopic cholecystectomy. The patient, a 50-year-old male with a history of biliary colic, underwent a meticulous laparoscopy exploration revealing an undistended gallbladder with an unexpected yellowish tissue fragment resembling pancreatic parenchyma.
Clinical discussion
EPT has an incidence ranging from 0.55 % to 13.7 % in autopsy studies. While the origins of EPT remain unclear, theories regarding the embryonic separation of pancreatic tissue offer insights into its origins and displacement from the original site. Macroscopically, EPT may present as polypoid lesions or yellow nodules and is typically asymptomatic. The various attachment locations and potential manifestations in other intra-abdominal sites add complexity to its diagnosis. Imaging techniques are often ineffective, making histopathological examination essential for diagnosis.
Conclusion
Diagnosing EPT in the gallbladder before and during surgery often presents significant challenges. Pathologists should be aware of this rare incidental finding, as it can mimic a tumor and lead to an overdiagnosis of malignancy. Only a precise histopathologic examination can provide a definite diagnosis and distinguish it from malignancies. Laparoscopic cholecystectomy is sufficing treatment.


胆囊中的异位胰腺组织:胆囊切除术标本中的罕见偶然发现--病例报告。
简介:异位胰腺组织(EPT)是一种罕见的先天性异常,其特征是胰腺组织位于异常位置,与胰腺分离,与胰腺没有任何解剖或血管联系。这种异常通常是在手术或尸检中偶然发现的。这一特点给外科医生带来了临床和放射学上的挑战,特别是在腹腔镜或开放式手术中。病例报告:这篇文章提出了一个令人信服的病例EPT,偶然发现在计划腹腔镜胆囊切除术。患者,50岁男性,有胆道绞痛病史,经过仔细的腹腔镜检查,发现胆囊未膨胀,有一个意想不到的类似胰腺实质的淡黄色组织碎片。临床讨论:EPT在尸检中的发病率为0.55% ~ 13.7%。虽然EPT的起源尚不清楚,但有关胰腺组织胚胎分离的理论为其起源和从原始位置移位提供了见解。宏观上,EPT可表现为息肉样病变或黄色结节,通常无症状。腹内其他部位的不同附着部位和潜在表现增加了其诊断的复杂性。成像技术往往是无效的,使组织病理学检查必不可少的诊断。结论:术前和术中胆囊EPT的诊断具有重要的挑战性。病理学家应该意识到这种罕见的偶然发现,因为它可以模拟肿瘤并导致恶性肿瘤的过度诊断。只有精确的组织病理学检查才能提供明确的诊断并将其与恶性肿瘤区分开来。腹腔镜胆囊切除术是足够的治疗方法。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
1.10
自引率
0.00%
发文量
1116
审稿时长
46 days

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


