Disitamab vedotin plus toripalimab in patients with locally advanced or metastatic urothelial carcinoma (RC48-C014): a phase Ib/II dose-escalation and dose-expansion study
IF 56.7
1区 医学
Q1 ONCOLOGY
引用次数: 0
Abstract
Background
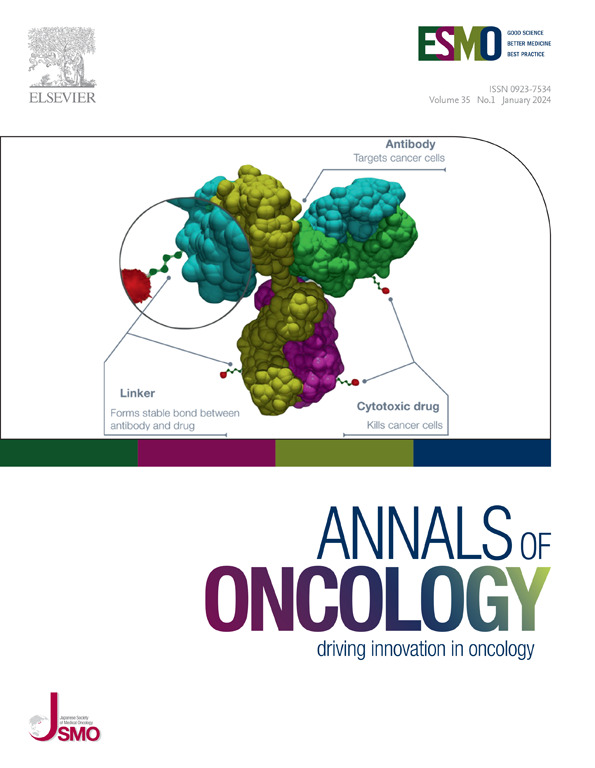
Human epidermal growth factor receptor 2 (HER2)-targeted antibody–drug conjugates (ADCs) such as disitamab vedotin (DV) and trastuzumab deruxtecan (T-DXd) have emerged as effective treatment options and received regulatory approvals for HER2-expressing locally advanced or metastatic urothelial carcinoma (la/mUC). In addition, ADCs in combination with immunotherapy have demonstrated antitumor activity. The current study aimed to evaluate the combination of DV and toripalimab in patients with la/mUC.
Patients and methods
This open-label phase Ib/II study enrolled patients with untreated or chemo-refractory la/mUC. During the dose-escalation phase, DV was administered at escalating doses of 1.5 and 2.0 mg/kg in combination with toripalimab 3.0 mg/kg once every 2 weeks. Primary endpoints were safety and the recommended phase II dose (RP2D). Secondary endpoints included objective response rate (ORR), progression-free survival (PFS), and overall survival (OS).
Results
From August 2020 to December 2021, a total of 41 patients were enrolled, including 6 in the dose-escalation phase and 35 in the dose-expansion phase. Sixty-one percent of patients were treatment naive. No dose-limiting toxicity was observed. The RP2D was determined as DV (2.0 mg/kg) plus toripalimab (3.0 mg/kg). By the data cut-off date of 1 March 2024, the confirmed ORR was 73.2%. The median PFS was 9.3 months, and the median OS was 33.1 months. The most common treatment-related adverse events (TRAEs) were aspartate aminotransferase increased (65.9%), alanine aminotransferase increased (63.4%), and peripheral sensory neuropathy (63.4%). Grade 3 or higher TRAEs occurred in 51.2% of patients, with the most common being γ-glutamyltransferase increased (12.2%), asthenia (9.8%), and alanine aminotransferase increased (7.3%). One treatment-related death (due to pneumonitis) was reported.
Conclusions
The combination of DV and toripalimab demonstrated promising response rate and OS results with a manageable safety profile in HER2-unselected la/mUC patients. This combination represents a promising first-line option for la/mUC. Randomized phase III study is currently ongoing.
双西他单维多汀联合托利哌单抗治疗局部晚期或转移性尿路上皮癌(RC48-C014):一项1b/2期剂量递增和剂量扩大研究
背景:HER2靶向抗体-药物偶联物(adc),如双西他单抗维多汀(DV)和曲妥珠单抗德鲁西替康(T-Dxd)已经成为治疗HER2表达局部晚期或转移性尿路上皮癌(la/mUC)的有效选择,并获得监管部门批准。此外,adc与免疫疗法联合使用已显示出抗肿瘤活性。目前的研究旨在评估DV和托利单抗在la/mUC患者中的联合应用。患者和方法:这项开放标签1b/2期研究纳入了未经治疗或化疗难治性la/mUC患者。在剂量递增阶段,DV以1.5和2.0 mg/kg的递增剂量与toripalimab 3.0 mg/kg联合施用,每两周一次。主要终点是安全性和推荐的2期剂量(RP2D)。次要终点包括客观缓解率(ORR)、无进展生存期(PFS)和总生存期(OS)。结果:从2020年8月至2021年12月,共入组41例患者,其中6例处于剂量递增期,35例处于剂量扩展期。61%的患者接受了治疗naïve。未观察到剂量限制性毒性。RP2D测定为DV (2.0 mg/kg) + toripalimab (3.0 mg/kg)。截至2024年3月1日的数据截止日期,确认的ORR为73.2%。中位PFS为9.3个月,中位OS为33.1个月。最常见的治疗相关不良事件(TRAEs)为天冬氨酸转氨酶升高(65.9%)、丙氨酸转氨酶升高(63.4%)和周围感觉神经病变(63.4%)。3级及以上trae发生在51.2%的患者中,最常见的是γ -谷氨酰转移酶升高(12.2%),虚弱(9.8%)和丙氨酸转氨酶升高(7.3%)。报告了一例治疗相关死亡(由于肺炎)。结论:在HER2未选择的la/mUC患者中,DV和托利哌单抗联合治疗显示出良好的缓解率和总生存率,并且具有可管理的安全性。这种组合代表了la/mUC的一线选择。随机III期研究目前正在进行中。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Annals of Oncology
医学-肿瘤学
CiteScore
63.90
自引率
1.00%
发文量
3712
审稿时长
2-3 weeks
期刊介绍:
Annals of Oncology, the official journal of the European Society for Medical Oncology and the Japanese Society of Medical Oncology, offers rapid and efficient peer-reviewed publications on innovative cancer treatments and translational research in oncology and precision medicine.
The journal primarily focuses on areas such as systemic anticancer therapy, with a specific emphasis on molecular targeted agents and new immune therapies. We also welcome randomized trials, including negative results, as well as top-level guidelines. Additionally, we encourage submissions in emerging fields that are crucial to personalized medicine, such as molecular pathology, bioinformatics, modern statistics, and biotechnologies. Manuscripts related to radiotherapy, surgery, and pediatrics will be considered if they demonstrate a clear interaction with any of the aforementioned fields or if they present groundbreaking findings.
Our international editorial board comprises renowned experts who are leaders in their respective fields. Through Annals of Oncology, we strive to provide the most effective communication on the dynamic and ever-evolving global oncology landscape.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


