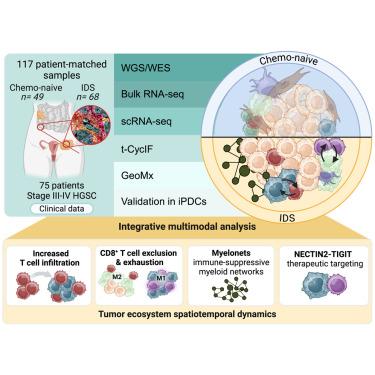
Chemotherapy induces myeloid-driven spatially confined T cell exhaustion in ovarian cancer
IF 48.8
1区 医学
Q1 CELL BIOLOGY
引用次数: 0
Abstract
Anti-tumor immunity is crucial for high-grade serous ovarian cancer (HGSC) prognosis, yet its adaptation upon standard chemotherapy remains poorly understood. Here, we conduct spatial and molecular characterization of 117 HGSC samples collected before and after chemotherapy. Our single-cell and spatial analyses reveal increasingly versatile immune cell states forming spatiotemporally dynamic microcommunities. We describe Myelonets, networks of interconnected myeloid cells that contribute to CD8+ T cell exhaustion post-chemotherapy and show that M1/M2 polarization at the tumor-stroma interface is associated with CD8+ T cell exhaustion and exclusion, correlating with poor chemoresponse. Single-cell and spatial transcriptomics reveal prominent myeloid-T cell interactions via NECTIN2-TIGIT induced by chemotherapy. Targeting these interactions using a functional patient-derived immuno-oncology platform demonstrates that high NECTIN2-TIGIT signaling in matched tumors predicts responses to immune checkpoint blockade. Our discovery of clinically relevant myeloid-driven spatial T cell exhaustion unlocks immunotherapeutic strategies to unleash CD8+ T cell-mediated anti-tumor immunity in HGSC.
求助全文
约1分钟内获得全文
求助全文
来源期刊
Cancer Cell
医学-肿瘤学
CiteScore
55.20
自引率
1.20%
发文量
179
审稿时长
4-8 weeks
期刊介绍:
Cancer Cell is a journal that focuses on promoting major advances in cancer research and oncology. The primary criteria for considering manuscripts are as follows:
Major advances: Manuscripts should provide significant advancements in answering important questions related to naturally occurring cancers.
Translational research: The journal welcomes translational research, which involves the application of basic scientific findings to human health and clinical practice.
Clinical investigations: Cancer Cell is interested in publishing clinical investigations that contribute to establishing new paradigms in the treatment, diagnosis, or prevention of cancers.
Insights into cancer biology: The journal values clinical investigations that provide important insights into cancer biology beyond what has been revealed by preclinical studies.
Mechanism-based proof-of-principle studies: Cancer Cell encourages the publication of mechanism-based proof-of-principle clinical studies, which demonstrate the feasibility of a specific therapeutic approach or diagnostic test.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


