Comparative effects of ciprofol and propofol on perioperative outcomes: a systematic review and meta-analysis of randomized controlled trials
IF 1.9
4区 医学
Q2 ANESTHESIOLOGY
引用次数: 0
Abstract
Background
The ideal anesthetic agents for sedation, considering their respiratory and cardiovascular benefits and other perioperative or postoperative outcomes, are still unclear. This systematic review and meta-analysis aimed to evaluate whether ciprofol has advantages over propofol for sedation, particularly concerning respiratory and cardiovascular outcomes and other relevant perioperative measures.
Methods
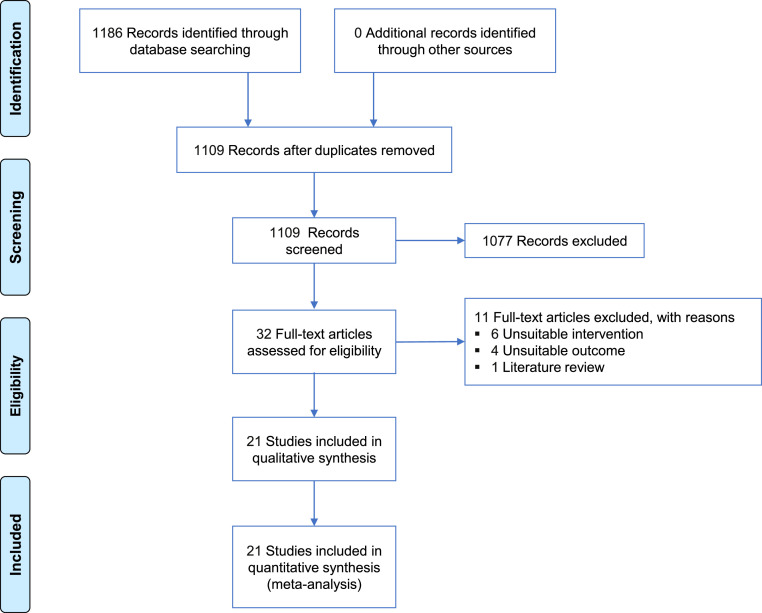
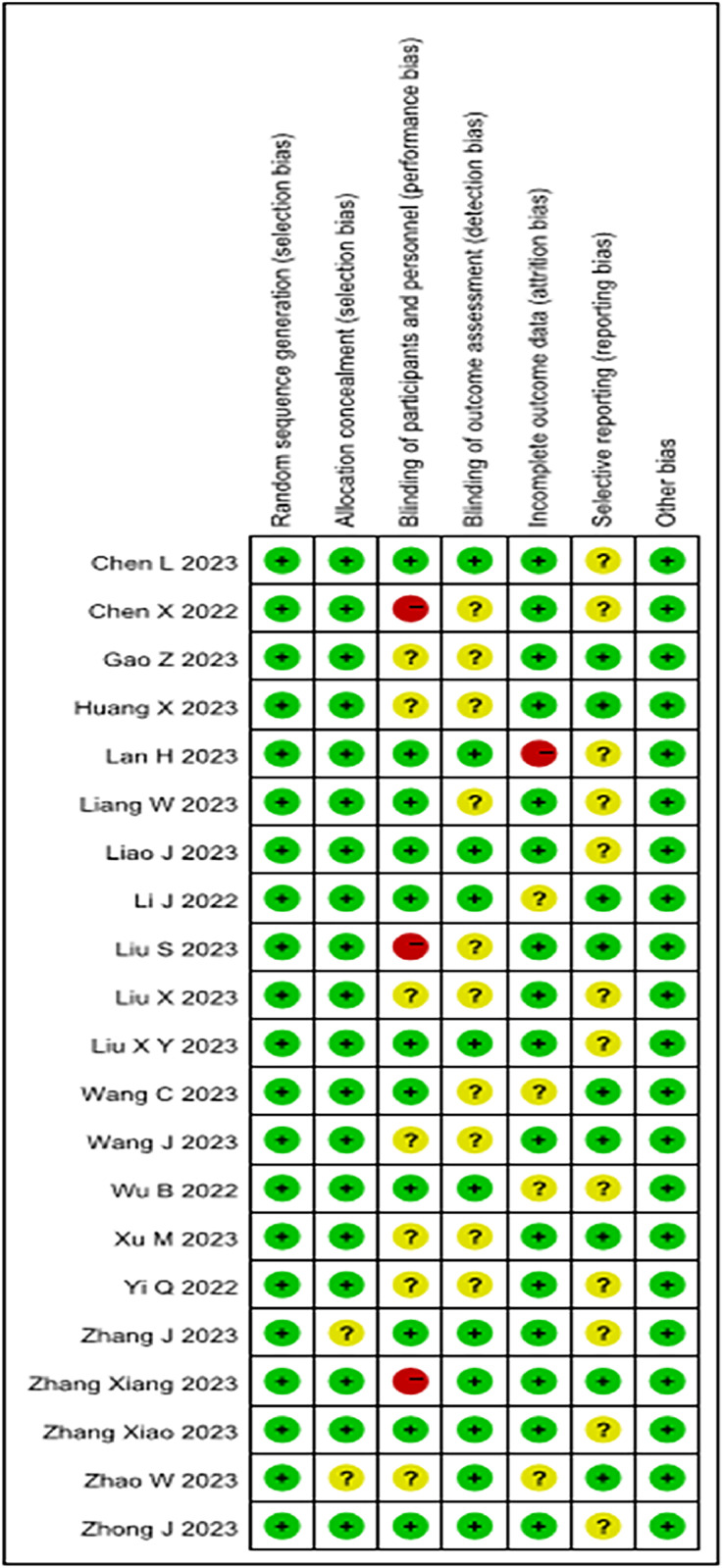
We conducted a comprehensive search of PubMed, Web of Science, the Cochrane Central Register of Controlled Trials, and two Chinese databases for randomized controlled trials comparing intravenous ciprofol and propofol for sedation. The primary outcome was the incidence of adverse respiratory events. Secondary outcomes included incidences of injection pain, hypotension, hypertension, bradycardia during surgery, perioperative nausea and vomiting, and postoperative awakening time. A random-effects model was used for more than four studies; otherwise, we employed the random-effects model with the Hartung-Knapp-Sidik-Jonkman adjustment.
Results
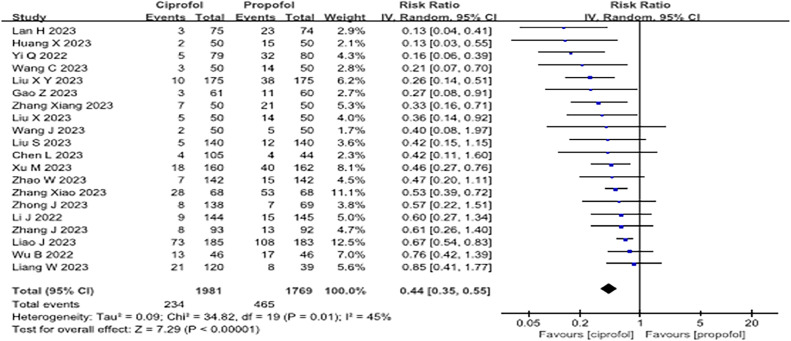
Intravenous ciprofol resulted in fewer adverse respiratory events than propofol (Risk Ratio [RR = 0.44]; 95% Confidence Interval [95% CI 0.35–0.55], p < 0.001, I2 = 45%, low quality). It also showed a lower incidence of injection pain (RR = 0.12; 95% CI 0.08‒0.17, p < 0.001, I2 = 36%, low quality), intraoperative hypotension (RR = 0.64; 95% CI 0.52–0.77, p < 0.001, I2 = 58%, low quality), and nausea and vomiting than propofol (RR = 0.67; 95% CI 0.49–0.92; p = 0.01, I2 = 0%, moderate quality). However, no significant differences were observed for hypertension, bradycardia, and awakening time.
Conclusions
Ciprofol may be more effective than propofol in minimizing perioperative respiratory adverse events and maintaining hemodynamic stability during sedation without prolonging recovery time.
环丙酚和异丙酚对围手术期预后的比较影响:随机对照试验的系统回顾和荟萃分析。
背景:考虑到其呼吸和心血管方面的益处以及其他围手术期或术后结局,理想的镇静麻醉剂仍不清楚。本系统综述和荟萃分析旨在评估环丙酚在镇静方面是否优于异丙酚,特别是在呼吸和心血管结局以及其他相关围手术期措施方面。方法:我们对PubMed、Web of Science、Cochrane Central Register of Controlled Trials和两个中文随机对照试验数据库进行了全面检索,比较静脉注射环丙酚和异丙酚的镇静作用。主要结局是不良呼吸事件的发生率。次要结局包括注射疼痛、低血压、高血压、术中心动过缓、围术期恶心呕吐和术后苏醒时间的发生率。四项以上的研究使用了随机效应模型;否则,我们采用Hartung-Knapp-Sidik-Jonkman平差的随机效应模型。结果:静脉注射环丙酚的不良呼吸事件发生率低于异丙酚(风险比[RR = 0.44];95%置信区间[95% CI 0.35-0.55], p < 0.001, I2 = 45%,低质量)。注射痛发生率较低(RR = 0.12;95% CI 0.08-0.17, p < 0.001, I2 = 36%,低质量)、术中低血压(RR = 0.64;95% CI 0.52-0.77, p < 0.001, I2 = 58%,低质量),且恶心呕吐优于异丙酚(RR = 0.67;95% ci 0.49-0.92;p = 0.01,I2 = 0%,质量中等)。然而,在高血压、心动过缓和觉醒时间方面没有观察到显著差异。结论:环丙酚可能比异丙酚更有效地减少围手术期呼吸不良事件和维持镇静期间血流动力学稳定,而不延长恢复时间。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Brazilian Journal of Anesthesiology
ANESTHESIOLOGY-
CiteScore
2.10
自引率
0.00%
发文量
88
审稿时长
68 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


