Association between coagulation activity and clinical and imaging outcomes in acute ischemic stroke patients - A sub-study of the MR CLEAN NO-IV trial
IF 3.7
3区 医学
Q1 HEMATOLOGY
引用次数: 0
Abstract
Background
The MR CLEAN NO-IV trial showed neither superiority nor noninferiority of endovascular treatment (EVT) alone compared to intravenous thrombolysis (IVT; Alteplase) before EVT in acute ischemic stroke (AIS) patients with large vessel occlusion of the anterior circulation. Although the treatment effect is largely attributable to EVT, IVT may affect hypercoagulability during AIS.
Aims
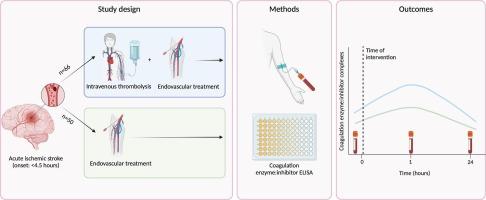
To investigate the association between activated coagulation and final infarct volume and clinical outcomes (modified Rankin Scale 3–6 and mortality 90 days post-EVT), and whether this effect is modified by IVT administration.
Methods
Enzyme-linked immunosorbent assays were used to quantify activated coagulation markers (activated coagulation factor (F) XIIa-C1 esterase inhibitor (C1inh); FXIIa-antithrombin (AT), FXIa-C1inh, FXIa-AT, FIXa-AT, FXa-AT, T-AT, FVIIa-AT) in plasma samples obtained on admission (T0), 1 h post-EVT (T1) and 24 h post-EVT (T2). Multivariable regressions were performed to investigate the associations and effect modification.
Results
In the total cohort of 116 patients, a significant increase at T1 was seen in FIXa-AT (p = .001), FXa-AT (p < .001), T-AT (p < .001), and FVIIa-AT (p = .012), while there was a significant increase at T2 in FXIIa-C1inh (p < .001). Similar results were seen in the IVT+EVT subgroup. The EVT alone subgroup showed a significant temporary increase at T1 in FXa-AT (p < .001) and T-AT (p = .014). Neither the enzyme:inhibitor complexes nor the interaction with IVT were significantly associated with the outcome measures.
Conclusion
Despite temporary significant increases in enzyme:inhibitor complexes in the IVT+EVT group, but not in the EVT alone group, there were no significant associations with final infarct volume and clinical outcomes.
急性缺血性脑卒中患者凝血活动与临床和影像学结果之间的关系--MR CLEAN NO-IV 试验的一项子研究。
背景:MR CLEAN NO-IV试验显示,在前循环大血管闭塞的急性缺血性卒中(AIS)患者中,单纯血管内治疗(EVT)与EVT前静脉溶栓(IVT;Alteplase)相比既无优势也无劣势。目的:研究活化凝血与最终梗死体积和临床结局(改良Rankin量表3-6和EVT后90天的死亡率)之间的关系,以及IVT的应用是否会改变这种影响:采用酶联免疫吸附试验定量检测入院时(T0)、EVT后1小时(T1)和EVT后24小时(T2)血浆样本中的活化凝血标志物(活化凝血因子(F)XIIa-C1酯酶抑制剂(C1inh)、FXIIa-抗凝血酶(AT)、FXIa-C1inh、FXIa-AT、FIXa-AT、FXa-AT、T-AT、FVIIa-AT)。研究人员对这些数据进行了多变量回归,以探讨其关联性和效应修正:尽管在 IVT+EVT 组中,酶:抑制剂复合物暂时明显增加,而在单独 EVT 组中则没有,但这与最终梗死体积和临床预后没有明显关联。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Thrombosis research
医学-外周血管病
CiteScore
14.60
自引率
4.00%
发文量
364
审稿时长
31 days
期刊介绍:
Thrombosis Research is an international journal dedicated to the swift dissemination of new information on thrombosis, hemostasis, and vascular biology, aimed at advancing both science and clinical care. The journal publishes peer-reviewed original research, reviews, editorials, opinions, and critiques, covering both basic and clinical studies. Priority is given to research that promises novel approaches in the diagnosis, therapy, prognosis, and prevention of thrombotic and hemorrhagic diseases.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


