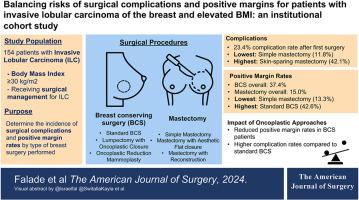
Balancing risks of surgical complications and positive margins for patients with invasive lobular carcinoma of the breast and elevated BMI: An institutional cohort study
IF 2.7
3区 医学
Q1 SURGERY
引用次数: 0
Abstract
Background
The risks of postoperative complications in breast cancer patients vary by patient and tumor characteristics. Elevated BMI and invasive lobular carcinoma (ILC) increase risks of surgical complications and positive margins, respectively.
Methods
We retrospectively analyzed patients with BMI ≥30 kg/m2 from an institutional ILC database. The primary outcome was surgical complication rate by procedure type. The secondary outcome was positive margin rates by surgical approach, stratified by T stage.
Results
Of 154 analyzed patients, standard BCS, lumpectomy with oncoplastic closure, and simple mastectomy had the lowest complication rates (18.2 %, 17.0 %, 11.8 %). Oncoplastic reduction mammoplasty and mastectomy with aesthetic closure had the highest rates (35.5 %, 33.3 %). The overall positive margin rate was 28.5 %, significantly higher in BCS vs. mastectomy (37.4 % vs. 15.0 %, p = 0.003). Oncoplastic surgery significantly reduced positive margin rates in BCS.
Conclusion
In this study, 23.4 % of patients experienced surgical complications, with higher rates in oncoplastic/reconstructive approaches. However, oncoplastic surgery reduced positive margins, highlighting the importance of balancing risks for optimal surgical planning.
平衡乳腺浸润性小叶癌患者手术并发症和边缘阳性的风险:一项机构队列研究。
背景:乳腺癌患者术后并发症的风险因患者和肿瘤特征而异。体重指数(BMI)升高和浸润性小叶癌(ILC)分别会增加手术并发症和边缘阳性的风险:我们回顾性分析了机构 ILC 数据库中体重指数≥30 kg/m2 的患者。主要结果是手术类型的手术并发症发生率。次要结果是按T期分层的手术方式的阳性边缘率:结果:在分析的 154 名患者中,标准 BCS、带肿瘤整形闭合的肿块切除术和单纯乳房切除术的并发症发生率最低(18.2%、17.0%、11.8%)。肿瘤整形缩小乳房成形术和乳房切除加美学闭合术的并发症发生率最高(35.5%、33.3%)。总的阳性边缘率为 28.5%,BCS 与乳房切除术相比明显更高(37.4% 对 15.0%,P = 0.003)。肿瘤整形手术大大降低了BCS的边缘阳性率:结论:在这项研究中,23.4%的患者出现了手术并发症,肿瘤整形/重建方法的并发症发生率更高。然而,肿瘤整形手术降低了阳性边缘率,突出了平衡风险对最佳手术规划的重要性。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
5.00
自引率
6.70%
发文量
570
审稿时长
56 days
期刊介绍:
The American Journal of Surgery® is a peer-reviewed journal designed for the general surgeon who performs abdominal, cancer, vascular, head and neck, breast, colorectal, and other forms of surgery. AJS is the official journal of 7 major surgical societies* and publishes their official papers as well as independently submitted clinical studies, editorials, reviews, brief reports, correspondence and book reviews.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


