Management of people after stroke in 383 Victorian general practices, 2014–2018: analysis of linked stroke registry and general practice data
Abstract
Objective
To evaluate the management in Victorian general practice of people who have been hospitalised with stroke or transient ischaemic attacks (TIA).
Study design
Retrospective observational study; analysis of linked Australian Stroke Clinical Registry (AuSCR) and general practice data.
Setting
383 general practices in the Eastern Melbourne, South Eastern Melbourne, and Gippsland primary health networks (Victoria), 1 January 2014 – 31 December 2018.
Participants
Adults who had been hospitalised with acute stroke or TIA and had at least two encounters with the same general practice during the observation period (7–18 months after the acute event).
Main outcome measures
Assessment of cardiometabolic risk factors (blood pressure, serum lipids, blood glucose, urinary protein); prescribing of guideline-recommended prevention medications (blood pressure-, lipid-, or glucose-lowering, antithrombotic agents); attainment of guideline targets for cardiometabolic risk factors at final assessment during observation period.
Results
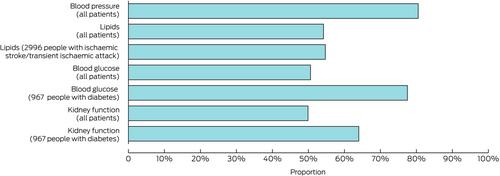
During 2014–2018, 3376 eligible AuSCR registrants (1465 women, 43.4%) had at least two encounters with one of the 383 general practices during the observation period; median age at stroke onset was 73.9 (interquartile range, 64.4–81.9) years, 737 events were TIAs (21.8%). Blood pressure was assessed in 2718 patients (80.5%), serum lipids in 1830 (54.2%), blood glucose in 1708 (50.6%). Prevention medications were prescribed for 2949 patients (87.4%), including lipid-lowering (2427, 71.9%) and blood pressure-lowering agents (2363, 70.0%). Blood glucose targets had been achieved by 1346 of 1708 patients assessed for this risk factor (78.8%), blood pressure targets by 1935 of 2717 (71.2%), and serum lipid targets by 765 of 1830 (41.8%). The incidence of having risk factors assessed was lower among patients aged 60 years or younger (incidence rate ratio [IRR], 0.97; 95% confidence interval [CI], 0.92–1.03) and those over 80 years of age (IRR, 0.92; 95% CI 0.88–0.97) than for those aged 61–80 years, and for women (IRR, 0.91; 95% CI, 0.87–0.95) and people with dementia (IRR, 0.89; 95% CI, 0.81–0.98). The likelihood of having classes of prevention medication prescribed was lower for patients aged 60 years or younger (IRR, 0.92; 95% CI, 0.88–0.97) and those over 80 years of age (IRR, 0.96; 95% CI, 0.92–0.997) than for patients aged 61–80 years, and for women (IRR, 0.95; 95% CI, 0.91–0.98) and people with dementia (IRR, 0.88; 95% CI, 0.78–0.98).
Conclusions
The general practice management of people who have been hospitalised with stroke or TIA could be improved. Effective monitoring of cardiometabolic risk factors will enable general practitioners to optimise care for people who need careful attention to prevent adverse secondary events.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


