Association of alcohol with lung cancer risk in men with different growth hormone receptor genotypes
IF 4.5
2区 医学
Q1 ONCOLOGY
引用次数: 0
Abstract
Objective
To test whether genetic variants of the growth hormone receptor gene (GHR) modulate the effect of lifestyle variables on lung cancer (LC) risk.
Materials and methods
This population-based cohort study involved 6,439 men from the Japan-Hawaii Cancer study drawn from the Kuakini Honolulu Heart Program who were cancer-free at baseline examination (1965–1968; age 45–68 years) and followed-up until December 1999. We determined the association of GHR SNP rs4130113 genotypes GHR-AA (common allele A homozygotes) and GHR-G (minor allele G carriage) with alcohol drinking, BMI, physical activity and cigarette smoking in relation to LC and non-small cell LC (NSCLC). Results were expressed as hazard ratios and 95 % CIs estimated from Cox proportional hazard models.
Results
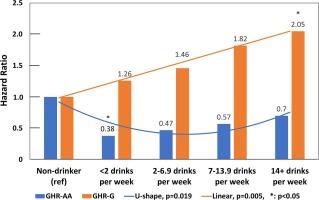
Over mean 26.7 ± 7.4 SD years follow-up, 190 LC cases, including 133 NSCLC cases, were diagnosed. After adjusting for age, education, alcohol intake, BMI, physical activity, cigarette smoking, green tea consumption and dietary saturated fat, main-effect Cox models showed that compared with GHR-AA, GHR-G was associated with protection against LC: HR = 0.75 (95 % CI, 0.56–1.00). Full Cox models showed GHR-G interacted with alcohol intake only (β = 1.171; p = 0.0003; drinks per week: β = 0.279; P = 0.0024). Stratified analyses showed that for GHR-AA, drinkers had reduced LC risk (HR = 0.54; 95 % CI, 0.35–0.85), and that <2 drinks/week had the strongest protection (HR = 0.38; 95 % CI, 0.18–0.83). In contrast, for GHR-G, alcohol drinkers had increased LC risk (HR = 1.70; 95 % CI, 1.07–2.69) which was dose-dependent (P for trend = 0.005). Results for NSCLC were similar.
Conclusion
In men with the GHR-AA genotype, alcohol drinking at a low dose poses significantly less risk of LC compared with non-drinkers and higher alcohol consumption., the overall relationship being U-shaped. In contrast, in GHR minor allele carriers, alcohol posed a progressively greater risk of LC as amount consumed increased.
酒精与不同生长激素受体基因型男性患肺癌风险的关系。
目的:检测生长激素受体基因的遗传变异是否会调节生活方式变量对肺癌风险的影响:检验生长激素受体基因(GHR)的遗传变异是否会调节生活方式变量对肺癌(LC)风险的影响:这项基于人群的队列研究涉及日本-夏威夷癌症研究中的 6439 名男性,他们来自 Kuakini 檀香山心脏计划,在基线检查(1965-1968 年;年龄 45-68 岁)时未患癌症,随访至 1999 年 12 月。我们确定了 GHR SNP rs4130113 基因型 GHR-AA(普通等位基因 A 的同卵双生者)和 GHR-G(小等位基因 G 的携带者)与饮酒、体重指数、体力活动和吸烟与 LC 和非小细胞 LC(NSCLC)的关系。结果以Cox比例危险模型估计的危险比和95 % CIs表示:在平均 26.7 ± 7.4 SD 年的随访期间,共诊断出 190 例 LC,其中包括 133 例 NSCLC。在对年龄、教育程度、酒精摄入量、体重指数、体力活动、吸烟、绿茶摄入量和膳食饱和脂肪进行调整后,主效应 Cox 模型显示,与 GHR-AA 相比,GHR-G 与预防 LC 相关:HR = 0.75(95 % CI,0.56-1.00)。完全 Cox 模型显示,GHR-G 仅与酒精摄入量存在交互作用(β = 1.171;P = 0.0003;每周饮酒量:β = 0.279;P = 0.0024)。分层分析表明,GHR-AA 饮酒者的 LC 风险降低(HR = 0.54;95 % CI,0.35-0.85),结论是:GHR-AA 饮酒者的 LC 风险降低(HR = 0.54;95 % CI,0.35-0.85):在具有 GHR-AA 基因型的男性中,与不饮酒者和饮酒量较高者相比,低剂量饮酒导致 LC 的风险明显降低,总体关系呈 U 型。与此相反,在 GHR 小等位基因携带者中,随着饮酒量的增加,患 LC 的风险逐渐增大。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Lung Cancer
医学-呼吸系统
CiteScore
9.40
自引率
3.80%
发文量
407
审稿时长
25 days
期刊介绍:
Lung Cancer is an international publication covering the clinical, translational and basic science of malignancies of the lung and chest region.Original research articles, early reports, review articles, editorials and correspondence covering the prevention, epidemiology and etiology, basic biology, pathology, clinical assessment, surgery, chemotherapy, radiotherapy, combined treatment modalities, other treatment modalities and outcomes of lung cancer are welcome.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


