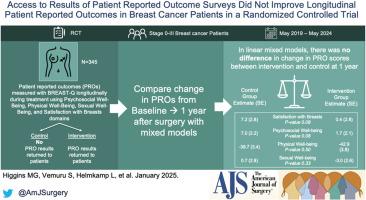
Access to results of patient reported outcome surveys did not improve longitudinal patient reported outcomes in breast cancer patients in a randomized controlled trial
IF 2.7
3区 医学
Q1 SURGERY
引用次数: 0
Abstract
Background
We assessed the impact of breast cancer (BC) patients receiving their own patient-reported outcome (PRO) results on future PROs.
Methods
Newly diagnosed female BC patients completed validated measures of satisfaction with breasts (SB), and psychosocial (PsyW), physical (PhW), and sexual wellbeing (SW) longitudinally during treatment. Patients were randomized to receive their PRO scores (Intervention) or not (Control). The primary outcome was difference in PRO scores from baseline to 1-year post-surgery. T- and chi2-tests compared baseline characteristics between groups. Linear mixed models assessed differences in PRO changes over time.
Results
131 patients (70 intervention, 61 control) completed baseline and 1-year modules; groups were well-balanced. At 1-year, the intervention group had less improvement in PsyW compared to controls with a t-test (mean difference: 1.2 vs 8.3, p = 0.04); this difference did not remain in mixed models (intervention group effect estimate (SE) 1.7 (2.1) vs control group 7.0 (2.2), p = 0.08). Changes in SB, PhW, and SW did not differ.
Conclusions
Access to individual PRO scores throughout treatment did not improve BC patients’ future PROs.
在随机对照试验中,获取患者报告结果调查结果并不能改善乳腺癌患者的纵向患者报告结果
背景我们评估了乳腺癌(BC)患者接受自己的患者报告结果(PRO)对未来PROs的影响。方法新确诊的女性BC患者在治疗期间纵向完成了对乳房(SB)、社会心理(PsyW)、身体(PhW)和性健康(SW)满意度的有效测量。患者被随机分配到接受 PRO 评分(干预组)或不接受 PRO 评分(对照组)。主要研究结果是PRO评分从基线到术后1年的差异。T检验和chi2检验比较了组间的基线特征。线性混合模型评估了PRO随时间变化的差异。结果131名患者(70名干预组,61名对照组)完成了基线和1年模块;各组之间非常均衡。1 年时,经 t 检验,干预组与对照组相比,PsyW 的改善幅度较小(平均差异:1.2 vs 8.3,p = 0.04);在混合模型中,这一差异并未保持(干预组效应估计值 (SE) 1.7 (2.1) vs 对照组 7.0 (2.2),p = 0.08)。SB、PhW 和 SW 的变化没有差异。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
5.00
自引率
6.70%
发文量
570
审稿时长
56 days
期刊介绍:
The American Journal of Surgery® is a peer-reviewed journal designed for the general surgeon who performs abdominal, cancer, vascular, head and neck, breast, colorectal, and other forms of surgery. AJS is the official journal of 7 major surgical societies* and publishes their official papers as well as independently submitted clinical studies, editorials, reviews, brief reports, correspondence and book reviews.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


