Prospective Outcomes of Standardized Non-operative Management of Pancreatic Trauma With Ductal Injury in Children: Less is More
IF 2.4
2区 医学
Q1 PEDIATRICS
引用次数: 0
Abstract
Background
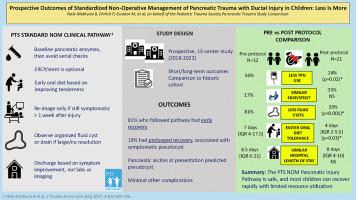
Traumatic pancreatic laceration with ductal injury in children can be managed non-operatively (NOM); however, variable management affects outcomes. We hypothesized that a standardized management approach with early feeding and limited resource utilization is safe and improves outcomes.
Method
Prospective, multicenter study of 13 pediatric trauma centers (2018–2022). Children with blunt pancreatic trauma with ductal injury were managed per a standard NOM pathway. Outcomes were compared to a historical NOM cohort with variable management.
Results
Of 22 patients, the median age was 7.5 years (range 1–14 years). Low-fat diet was started at median 4 days [IQR 2–7] and median hospital stay was 8 days [IQR 4–10]. One patient failed NOM and underwent distal pancreatectomy. Of the rest, most (17/21, 81%) had early recovery and discharged in median 6 days [IQR 4–8.25] while 4 (19%) had prolonged recovery (median stay 24 days, IQR 19.8–30.5) and higher peri-pancreatic cyst development (early 23.5% vs prolonged 75%,p = 0.05). Pancreatic ascites at presentation correlated with cyst development (p < 0.0001). Endoscopic stent (optional) was placed in 33% and did not prevent cyst development. Delayed exocrine pancreatic insufficiency was noted in 1 patient. Compared to the historic cohort (32 patients), TPN use was lower (pre-protocol 56% vs post 23%, p = 0.02), days to diet was shorter (pre-protocol 7 vs post 4; p = 0.03), and cyst development was lower (pre-protocol 81% vs post 33%, p < 0.001).
Conclusion
Children with traumatic pancreatic ductal injury can be safely managed per the PTS NOM clinical pathway and most recover rapidly. Pancreatic ascites may predict pseudocyst formation.
Levels of Evidence
IV. Study type: therapeutic, comparative.
儿童胰腺创伤伴导管损伤标准化非手术治疗的前瞻性结果:少即是多
背景:儿童外伤性胰腺裂伤伴导管损伤可采用非手术治疗(NOM),但不同的治疗方法会影响治疗效果。我们假设,早期喂养和有限资源利用的标准化管理方法既安全又能改善预后:13 个儿科创伤中心的前瞻性多中心研究(2018-2022 年)。钝性胰腺创伤伴导管损伤的患儿按照标准 NOM 路径进行管理。结果与历史上管理不一的NOM队列进行了比较:22名患者的中位年龄为7.5岁(1-14岁)。开始低脂饮食的时间中位数为 4 天[IQR 2-7],住院时间中位数为 8 天[IQR 4-10]。一名患者 NOM 失败,接受了远端胰腺切除术。其余患者中,大多数(17/21,81%)恢复较早,中位住院时间为 6 天[IQR 4-8.25],4 例(19%)恢复时间较长(中位住院时间为 24 天,IQR 19.8-30.5),胰周囊肿发生率较高(早期 23.5% 对长期 75%,P = 0.05)。发病时的胰腹水与囊肿的发展相关(p 结论:胰腺外伤性囊肿患儿的胰腺腹水与囊肿的发展相关:外伤性胰腺导管损伤患儿可根据 PTS NOM 临床路径进行安全处理,大多数患儿可迅速康复。胰腹水可预测假性囊肿的形成:IV.研究类型:治疗、比较。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
1.10
自引率
12.50%
发文量
569
审稿时长
38 days
期刊介绍:
The journal presents original contributions as well as a complete international abstracts section and other special departments to provide the most current source of information and references in pediatric surgery. The journal is based on the need to improve the surgical care of infants and children, not only through advances in physiology, pathology and surgical techniques, but also by attention to the unique emotional and physical needs of the young patient.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


