Changing Landscape of Open Offers in Liver Transplantation in the Machine Perfusion Era: Exposure, Equity, and Economics
Abstract
Background
Open offers (OOs) in liver transplantation (LT) result from bypassing the traditional allocation system. Little is known about the trends of OOs or the differences in donor/recipient characteristics compared to traditionally placed organs. We aim to quantify modern practices regarding OOs and understand NMP's impact, focusing on social determinants of health (SDH), cost, and graft-associated risk.
Methods
LTs from 1/1/2018 to 12/31/2023 at a single center were included. NMP was implemented on 10/1/2022. The CDC (centers for disease control)-validated social vulnerability index (SVI) and donor risk index (DRI) were calculated. Comprehensive complications index (CCI), Clavien-Dindo grades, patient and graft survival, and costs of transplantation were included.
Results
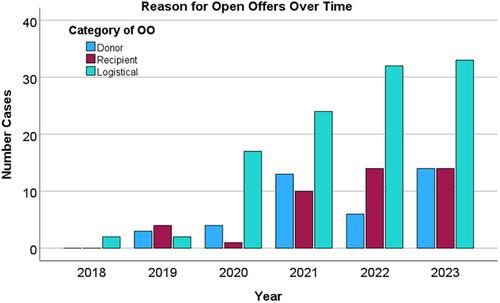
1162 LTs were performed; 193 (16.8%) from OOs. OOs were more common in the post-NMP era (26.5% vs. 13.3%, p < 0.001). Pre-NMP, patients receiving OOs had longer waitlist times (118 vs. 69 days, p < 0.001), lower MELDs (17 vs. 25 points, p < 0.001), and riskier grafts (DRI = 1.8 vs. 1.6, p = 0.004) compared to standard offers. Post-NMP, recipients receiving OOs demonstrated no difference in waitlist time (27 vs. 20 days, p = 0.21) or graft risk (DRI = 2.03 vs. 2.23, p = 0.17). OO recipient MELD remained lower (16 vs. 22, p < 0.001). OO recipients were more socially vulnerable (SVI), pre-NMP (0.41 vs. 0.36, p = 0.004), but less vulnerable after NMP (0.23 vs. 0.36, p = 0.019). Despite increased graft risk, pre-NMP OO-LTs were less expensive in the 90-day global period ($154 939 vs. $178 970, p = 0.002) and the 180-days pre-/post-LT ($208 807 vs. $228 091, p = 0.021). Cost trends remained similar with NMP.
Conclusion
OOs are increasingly utilized and may be appealing due to demonstrated cost reductions even with NMP. Although most OO-related metrics in our center remain similar before and after machine perfusion, programs should take caution that increasing use does not worsen organ access for socially vulnerable populations.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


