Mechanical complications and revision following total joint arthroplasty in acromegalic patients: A nationwide US-based study
IF 3.5
2区 医学
Q2 ENDOCRINOLOGY & METABOLISM
引用次数: 0
Abstract
Background
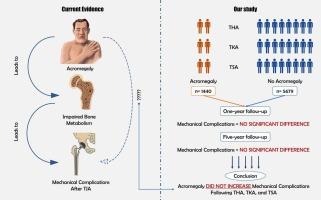
Acromegaly is associated with significant osteoarthritis (OA) and increased risk of vertebral and hip fractures. There is limited data on total joint arthroplasty (TJA) outcomes in patients with acromegaly.
Methods
In this retrospective study, we identified patients with acromegaly who underwent total hip arthroplasty (THA), total knee arthroplasty (TKA), and total shoulder arthroplasty (TSA) between 2010 and 2022 using the PearlDiver national database. Patients with a prior history of osteoporosis and follow-up duration of less than one year were excluded. Non-acromegalic control groups were selected through matching based on confounding factors. We compared all-cause revision and implant-related complications between the groups using R software integrated with the PearlDiver database.
Results
We identified 1440 patients with acromegaly: 665 underwent THA, 618 underwent TKA, and 157 underwent TSA. Compared to the control group (2634 THA, 2445 TKA, and 600 TSA), there was no significant association with post-op revision following THA (OR(1-year) = 0.76[0.42–1.28], OR(5-year) = 0.68[0.42–1.06]), TKA (OR(1-year) = 0.89[0.48–1.55], OR(5-year) = 0.78[0.49–1.17]), and TSA (OR(1-year) = 0.19[0.02–1.40], OR(5-year) = 0.32[0.10–1.07]). Additionally, the risk of mechanical complications did not significantly increase in patients with acromegaly, either one year or five years post-operation.
Conclusion
The study showed no significant increase in risk of revisions or mechanical complications in patients with acromegaly compared to controls. These findings bridge an important gap in the understanding of post-arthroplasty complications in patients with acromegaly and offer valuable insights into surgical expectations.
肢端肥大症患者全关节成形术后的机械并发症和翻修:一项基于美国的全国性研究。
背景:肢端肥大症与严重的骨关节炎(OA)以及椎骨和髋骨骨折风险增加有关。有关肢端肥大症患者接受全关节成形术(TJA)的结果的数据十分有限:在这项回顾性研究中,我们利用PearlDiver国家数据库确定了2010年至2022年间接受全髋关节置换术(THA)、全膝关节置换术(TKA)和全肩关节置换术(TSA)的肢端肥大症患者。排除了既往有骨质疏松症病史和随访时间少于一年的患者。根据混杂因素,通过配对筛选出非骨质疏松症对照组。我们使用集成了 PearlDiver 数据库的 R 软件比较了各组之间的全因翻修和植入相关并发症:我们确定了 1440 名肢端肥大症患者:其中 665 人接受了 THA 手术,618 人接受了 TKA 手术,157 人接受了 TSA 手术。与对照组(2634 例 THA、2445 例 TKA 和 600 例 TSA)相比,THA 术后翻修与肢端肥大症无明显关系(OR(1-year) = 0.76[0.42-1.28],OR(5 年)= 0.68[0.42-1.06])、TKA(OR(1 年)= 0.89[0.48-1.55],OR(5 年)= 0.78[0.49-1.17])和 TSA(OR(1 年)= 0.19[0.02-1.40],OR(5 年)= 0.32[0.10-1.07])与术后翻修无明显关联。此外,肢端肥大症患者发生机械并发症的风险在术后一年或五年内均无明显增加:该研究显示,与对照组相比,肢端肥大症患者发生翻修或机械并发症的风险没有明显增加。这些发现弥补了人们对肢端肥大症患者关节置换术后并发症认识上的一个重要空白,并为手术预期提供了有价值的见解。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Bone
医学-内分泌学与代谢
CiteScore
8.90
自引率
4.90%
发文量
264
审稿时长
30 days
期刊介绍:
BONE is an interdisciplinary forum for the rapid publication of original articles and reviews on basic, translational, and clinical aspects of bone and mineral metabolism. The Journal also encourages submissions related to interactions of bone with other organ systems, including cartilage, endocrine, muscle, fat, neural, vascular, gastrointestinal, hematopoietic, and immune systems. Particular attention is placed on the application of experimental studies to clinical practice.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


