Intensive care due to myasthenia gravis: Risk factors and prognosis
Abstract
Background and purpose
Exacerbation of myasthenia gravis (MG) with respiratory failure requires intensive care. We aimed to study the risk factors for intensive care unit admission for MG exacerbation and myasthenic crisis (MC) and the prognosis of people with MG (pwMG) thereafter.
Methods
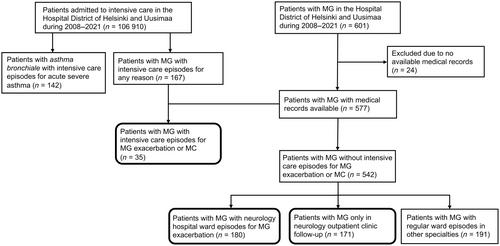
This retrospective study investigated patients in the Helsinki and Uusimaa hospital district during the years 2008–2021. PwMG (International Classification of Diseases, 10th revision code G70.0) were identified through a data repository search, followed by a chart review of patient records. Risk factors for intensive care due to MG exacerbation were evaluated as compared with the patients only treated in the outpatient clinic and those treated in the neurological ward for MG exacerbation. The outcomes of patients in intensive care for any reason were also compared with those of patients in intensive care for exacerbation of bronchial asthma.
Results
Of 577 pwMG, 35 (6.1%) needed intensive care for MG within a median of 5.3 months from diagnosis. The mean (±SD) age at MG diagnosis was higher in the intensive care group (60.5 [±16.1] years) compared to the outpatient (48.3 [±20.9] years; p < 0.001) and neurological ward groups (53.4 [±20.8] years; p = 0.044). Thymoma (odds ratio [OR] 4.8, 95% confidence interval [CI] 1.19–19.43; p = 0.028) and female sex (OR 2.1, 95% CI 1.02–4.48; p = 0.045) were independent risk factors for intensive care. In-hospital mortality was 4% for MC patients. Six-month mortality after intensive care for MG exacerbation (14.3%) was twice that for asthma exacerbation (7.7%).
Conclusion
Our study shows an increased risk of intensive care treatment for patients with late-onset MG, female sex or thymoma, occurring usually within 6 months from diagnosis, which emphasises the importance of early treatment choices.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


