Synergies between diabetes and hyperhomocysteinaemia: New insights to predict and prevent adverse cardiovascular effects
Abstract
Aim
To explore the association of hyperhomocysteinaemia (HHcy) and diabetes synergies with cardiovascular events in the adult population of northern China.
Methods
Data were collected from the Asymptomatic Polyvascular Abnomalities Community study for 2010 to 2019. Serum homocysteine (Hcy) levels were determined by enzyme-linked immunosorbent assay. The participants were categorized into four groups based on their Hcy levels and diabetes status: non-diabetes/non-HHcy, non-diabetes/HHcy, diabetes/non-HHcy and diabetes/HHcy. The composite endpoint consisted of the occurrence of first-ever stroke, myocardial infraction (MI) or all-cause mortality. Cox regression analyses were performed to evaluate the associations of diabetes and HHcy with cardiovascular disease (CVD) events.
Results
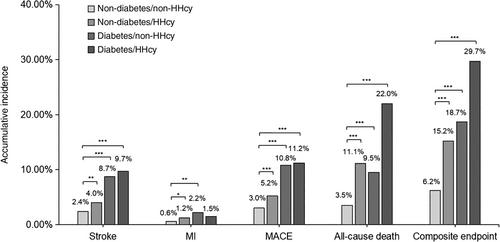
In total, 5278 participants were eligible (average age 55.1 years, 60% male). Over a follow-up of 9.1 years, 618 events were identified, 202 stroke, 52 MI and 406 all-cause deaths. Compared with the non-diabetes/non-HHcy group, hazard ratios with 95% confidence intervals in the diabetes/HHcy group for stroke, MI, major adverse cardiovascular event (MACE), all-cause death and composite endpoint were 1.85 (1.12-3.04), 1.33 (0.42-4.23), 1.78 (1.13-2.80), 2.24 (1.56-3.23) and 1.97 (1.47-2.65), respectively. Significant interactions between HHcy and diabetes status were found for stroke, MI and MACE (P for interaction = .002, .027 and .044, respectively). In addition, the association of diabetes/HHcy with stroke was modified by age (< 60 and ≥ 60 years; P for interaction = .016).
Conclusions
The findings highlight the synergistic impact of diabetes and HHcy on CVD. Joint assessments of diabetes and Hcy levels should be emphasized for risk stratification and primary prevention of CVD.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


