Impact of neonatal hyperoxia on adult cardiac autonomic function in rats: Role of angiotensin II type 1 receptor activation
IF 4.2
3区 医学
Q1 PHARMACOLOGY & PHARMACY
引用次数: 0
Abstract
Individuals born preterm present altered cardiac autonomic function, a risk factor to heart diseases. Neonatal renin-angiotensin-system activation contributes to adult cardiomyopathy in rats exposed to neonatal hyperoxia, a well-established model of preterm birth-related conditions. Central angiotensin II receptor activation is a key modulator of the autonomic drive to the heart. Whether neonatal hyperoxia leads to alteration of the cardiac autonomic function through activation of the angiotensin II receptor type 1 (AT1) is unknown and was examined in the present study.
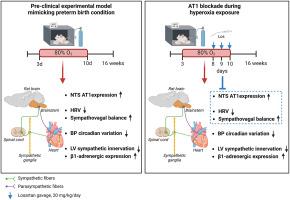
Sprague-Dawley pups were exposed to hyperoxia or room air from postnatal days 3–10. AT1 antagonist losartan or water was given orally postnatal days 8–10. Blood pressure, autonomic function, left ventricular sympathetic innervation, β-adrenergic-receptors expression, and AT1 expression in the solitary-tract-nucleus were examined in adult rats.
Neonatal hyperoxia led to loss of day-night blood pressure variation, decreased heart rate variability, increased sympathovagal balance, increased AT1 expression in the solitary-tract, decreased left ventricle sympathetic innervation, and increased β1-adrenergic-receptor protein expression. Losartan prevented the autonomic changes and AT1 expression in the solitary-tract but did not impact the loss of circadian blood pressure variation nor the changes in sympathetic innervation and in β1-adrenergic-receptor expression.
In conclusion, neonatal hyperoxia leads to both central autonomic and cardiac sympathetic changes, partly programmed by neonatal activation of the renin-angiotensin system.
新生儿高氧对大鼠成年心脏自主神经功能的影响:血管紧张素 II 1 型受体激活的作用
早产儿的心脏自主神经功能会发生改变,这是导致心脏病的一个危险因素。新生儿肾素-血管紧张素系统活化是导致大鼠患上成人心肌病的原因。中枢血管紧张素 II 受体激活是心脏自律神经驱动的一个关键调节器。新生儿高氧是否会通过激活血管紧张素 II 受体 1 型(AT1)而导致心脏自主神经功能的改变尚不清楚,本研究对此进行了研究。出生后第 8-10 天口服 AT1 拮抗剂洛沙坦或水。对成年大鼠的血压、自律神经功能、左心室交感神经支配、β肾上腺素能受体表达以及孤束核中AT1的表达进行了检测。新生儿高氧导致昼夜血压变化消失、心率变异性降低、交感-迷走平衡增加、孤束核中AT1表达增加、左心室交感神经支配减少以及β1肾上腺素能受体蛋白表达增加。总之,新生儿高氧会导致中枢自律神经和心脏交感神经的变化,其中部分原因是新生儿肾素-血管紧张素系统的激活。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
9.00
自引率
0.00%
发文量
572
审稿时长
34 days
期刊介绍:
The European Journal of Pharmacology publishes research papers covering all aspects of experimental pharmacology with focus on the mechanism of action of structurally identified compounds affecting biological systems.
The scope includes:
Behavioural pharmacology
Neuropharmacology and analgesia
Cardiovascular pharmacology
Pulmonary, gastrointestinal and urogenital pharmacology
Endocrine pharmacology
Immunopharmacology and inflammation
Molecular and cellular pharmacology
Regenerative pharmacology
Biologicals and biotherapeutics
Translational pharmacology
Nutriceutical pharmacology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


