Validation of ablation site classification accuracy and trends in the prediction of potential reconnection sites for atrial fibrillation using the CARTONET® R12.1 model
Abstract
Background
CARTONET® enables automatic ablation site classification and reconnection site prediction using machine learning. However, the accuracy of the site classification model and trends of the site prediction model for potential reconnection sites are uncertain.
Methods
We studied a total of 396 cases. About 313 patients underwent pulmonary vein isolation (PVI), including a cavotricuspid isthmus (CTI) ablation (PVI group) and 83 underwent PVI and additional ablation (i.e., box isolation) (PVI+ group). We investigated the sensitivity and positive predictive value (PPV) for automatic site classification in the total cohort and compared these metrics for PV lesions versus non-PV lesions. The distribution of potential reconnection sites and confidence level for each site was also investigated.
Results
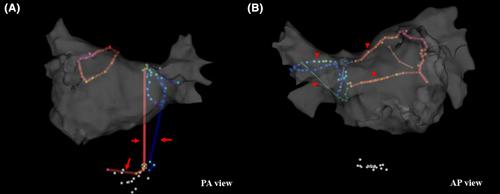
A total of 29,422 points were analyzed (PV lesions [n = 22 418], non-PV lesions [n = 7004]). The sensitivity and PPV of the total cohort were 71.4% and 84.6%, respectively. The sensitivity and PPV of PV lesions were significantly higher than those of non-PV lesions (PV lesions vs. non-PV lesions, %; sensitivity, 75.3 vs. 67.5, p < .05; PPV, 91.2 vs. 67.9, p < .05). CTI and superior vena cava could not be recognized or analyzed. In the potential reconnection prediction model, the incidence of potential reconnections was highest in the posterior, while the confidence was the highest in the roof.
Conclusion
The automatic site classification of the CARTONET®R12.1 model demonstrates relatively high accuracy in pulmonary veins excluding the carina. The prediction of potential reconnection sites feature tends to anticipate areas with poor catheter stability as reconnection sites.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


