Evaluation of an Australian community-based model of care for adults with intellectual and developmental disabilities undergoing procedures under sedation
Abstract
Background
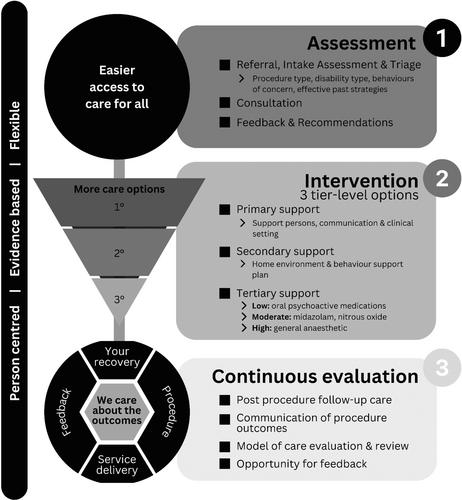
Adults with intellectual and developmental disabilities (IDDs) have higher healthcare needs, but experience difficulties accessing preventative healthcare. Despite this inequity, models of care that address barriers and provide customized treatment are limited, exacerbating vulnerabilities and poorer health outcomes. This study describes the development of a procedural model of care (PMOC) for adults with intellectual and developmental disabilities, and evaluates the sedation tier, exploring procedure and sedation outcomes.
Methods
Development of the PMOC was informed by current evidence and themes identified in stakeholder consultation and literature. A retrospective cohort study evaluated the sedation option within the model, conducted at a community-based disability service in Melbourne, Australia. All records over a 14-month period were included. Descriptive statistics and univariate logistic regression analysis were used to analyze data.
Results
The PMOC includes assessment, intervention, and evaluation tiers. Intervention options range from least to most invasive, culminating in the sedation level (mild; oral psychoactive, moderate; midazolam and nitrous oxide, high; general anesthetic). A total of 127 adults with IDDs received procedures under sedation; median age was 26 years, 61% lived with family, and 81% had multiple disabilities. A total of 197 procedures were referred to CDDH, including immunization (61%) and oral health reviews (23%), and resulted in 98% completion rate. Mild (n = 36) and moderate (n = 95) sedation were used for 67% of procedures. The PMOC correctly predicted 91% of sedation requirements. Living with family (OR 2.211, 95% CI 1.001–4.885, p = 0.05); immunization (OR 7.935, 95% CI 4.025–15.644, p <0.001); and multiple disabilities (OR 3.064, 95% CI 1.123–8.362, p = 0.029) were associated with mild, moderate and high sedation options, respectively.
Conclusions
Models of care offering individualized interventions can support adults with IDDs to receive preventative procedures. Demographic variables may be able to predict sedation requirements. Wider application of this model may reduce health inequity within this vulnerable population.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


