Necesidad de un protocolo de tratamiento antibiótico perioperatorio dirigido para pacientes con drenaje biliar preoperatorio intervenidos de duodenopancreatectomía cefálica
IF 1.3
4区 医学
Q3 SURGERY
引用次数: 0
Abstract
Purpose
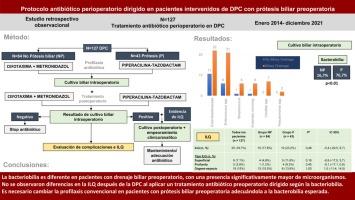
To evaluate the bacterobilia in patients undergoing pancreaticoduodenectomy (PD) based on whether they carry a preoperative biliary drainage or not and to analyse if a targeted perioperative antibiotic treatment based on the expected microbiology leads in no differences in Surgical Site Infections (SSI) between the groups.
Methods
Retrospective observational single-center study of patients undergoing pancreaticoduodenectomy with preoperative biliary stent (group P, Prosthesis) and without stent (group NP, No Prosthesis). Postoperative complications including SSI and its subtypes were analyzed after applying a targeted perioperative antibiotic treatment protocol with cefotaxime and metronidazole (group NP) and piperacillin-tazobactam (group P).
Results
Between January 2014 and December 2021, 127 patients were treated (84 in group NP and 43 in group P). Intraoperative cultures were positive in 16.7% (group NP) vs 76.7% (group P, P< .01). Microorganisms isolated in group NP included Enterobacterales (10.7%) and Enterococcus spp. (7.1%) with no Candida detected. In group P: Enterobacterales (51.2%), Enterococcus spp. (48.8%), and Candida (16.3%) were higher (P< .01%). No differences in morbidity and mortality were observed between the groups. SSI rate was 17.8% in group NP and 23.2% in group P (ns).
Conclusion
Bacterobilia differs in patients with biliary drainage, showing a higher presence of Enterobacterales, Enterococcus spp. and Candida. There were no differences in SSI incidence after applying perioperative antibiotic treatment tailored to the expected microorganisms in each group. This raises the need to reconsider conventional surgical prophylaxis in patients with biliary stent.
对接受头十二指肠切除术的术前胆汁引流患者实施有针对性的围手术期抗生素治疗方案的必要性
目的根据接受胰十二指肠切除术(PD)的患者术前是否携带胆道引流管评估其细菌嗜好,并分析根据预期的微生物学情况进行有针对性的围手术期抗生素治疗是否会导致两组患者的手术部位感染(SSI)无差异。方法对接受胰十二指肠切除术的患者进行单中心回顾性观察研究,研究对象为术前使用胆道支架的患者(P 组,支架)和不使用支架的患者(NP 组,无支架)。结果2014年1月至2021年12月,127名患者接受了治疗(NP组84人,P组43人),其中包括SSI及其亚型。16.7%(NP 组)与 76.7%(P 组,P< .01)的术中培养呈阳性。NP 组分离出的微生物包括肠杆菌属(10.7%)和肠球菌属(7.1%),未检出念珠菌。在 P 组中:肠杆菌属(51.2%)、肠球菌属(48.8%)和念珠菌属(16.3%)较高(P< .01%)。两组患者的发病率和死亡率无差异。NP 组的 SSI 感染率为 17.8%,P 组为 23.2%(ns)。各组患者在围手术期根据预期微生物使用抗生素治疗后,SSI 发生率并无差异。因此,有必要重新考虑胆道支架患者的常规手术预防措施。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Cirugia Espanola
SURGERY-
CiteScore
1.20
自引率
21.10%
发文量
173
审稿时长
53 days
期刊介绍:
Cirugía Española, an official body of the Asociación Española de Cirujanos (Spanish Association of Surgeons), will consider original articles, reviews, editorials, special articles, scientific letters, letters to the editor, and medical images for publication; all of these will be submitted to an anonymous external peer review process. There is also the possibility of accepting book reviews of recent publications related to General and Digestive Surgery.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


