Comparison of the clinical performance of the Ambu®AuraGain™ laryngeal mask in children undergoing surgery in the supine and prone position – A prospective, non-inferiority clinical trial
IF 5
2区 医学
Q1 ANESTHESIOLOGY
引用次数: 0
Abstract
Study objective
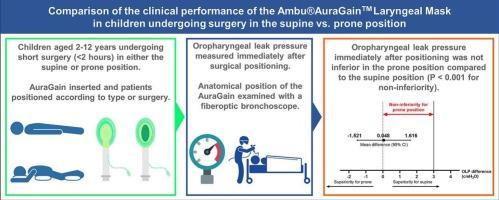
Reports are limited regarding supraglottic airway (SGA) usage in children in the prone position. This study aimed to compare the clinical performance of the Ambu®AuraGain™, a 2nd generation SGA, in children undergoing surgery in the prone and supine positions. We hypothesized that oropharyngeal leak pressure (OLP) in the prone position would not be inferior to that in the supine position.
Design
Single-center, prospective, non-randomized controlled study.
Setting
Operating room.
Patients
One hundred and twenty-six children, American Society of Anesthesiologists (ASA) physical status I-III, aged 2–12 years, undergoing elective surgery for 2 h or less in the supine or prone position.
Interventions
After induction of general anesthesia and insertion of the AuraGain, patients were positioned either supine or prone, according to type of surgery.
Measurements
OLP immediately after surgical positioning was measured as the primary outcome. The anatomical position of the AuraGain was evaluated using a flexible fiberoptic bronchoscope (Olympus LF-DP Tracheal Intubation Fiberscope, Melville, New York, USA). Airway maneuvers performed during placement and maintenance of the AuraGain and airway-related adverse events were recorded.
Main findings
The mean difference in OLP immediately after positioning was 0.048 cmH2O (95 % confidence interval: −1.521 to 1.616), and the non-inferiority hypothesis was accepted (P < 0.001 for non-inferiority). There was no significant difference in the anatomical position of the SGA and adverse events. Airway maneuvers were significantly more commonly performed during placement in the Prone group compared to the Supine group (51 (81.0 %) vs. 3 (4.8 %), respectively; P < 0.001).
Conclusion
OLP when using AuraGain in the prone position in children was not inferior to that in the supine position. This suggests that the AuraGain may be an effective option for children undergoing short surgical procedures in the prone position.
比较 Ambu®AuraGain™ 喉罩在儿童仰卧位和俯卧位手术中的临床表现 - 一项前瞻性、非劣效性临床试验
研究目的有关儿童俯卧位使用声门上气道(SGA)的报道很有限。本研究旨在比较第二代 SGA Ambu®AuraGain™ 在俯卧位和仰卧位接受手术的儿童中的临床表现。我们假设俯卧位的口咽漏压(OLP)不会低于仰卧位。设计单中心、前瞻性、非随机对照研究。干预措施诱导全身麻醉并插入 AuraGain 后,根据手术类型让患者仰卧或俯卧。使用柔性纤维支气管镜(Olympus LF-DP 气管插管纤维镜,美国纽约梅尔维尔)评估 AuraGain 的解剖位置。主要研究结果定位后即刻的 OLP 平均差异为 0.048 cmH2O(95 % 置信区间:-1.521 至 1.616),非劣效性假设成立(非劣效性 P < 0.001)。SGA 的解剖位置与不良事件无明显差异。与仰卧位组相比,俯卧位组在置管过程中更常进行气道操作(分别为 51 (81.0 %) vs. 3 (4.8 %);P < 0.001)。这表明,AuraGain 可能是儿童在俯卧位接受短手术的有效选择。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
7.40
自引率
4.50%
发文量
346
审稿时长
23 days
期刊介绍:
The Journal of Clinical Anesthesia (JCA) addresses all aspects of anesthesia practice, including anesthetic administration, pharmacokinetics, preoperative and postoperative considerations, coexisting disease and other complicating factors, cost issues, and similar concerns anesthesiologists contend with daily. Exceptionally high standards of presentation and accuracy are maintained.
The core of the journal is original contributions on subjects relevant to clinical practice, and rigorously peer-reviewed. Highly respected international experts have joined together to form the Editorial Board, sharing their years of experience and clinical expertise. Specialized section editors cover the various subspecialties within the field. To keep your practical clinical skills current, the journal bridges the gap between the laboratory and the clinical practice of anesthesiology and critical care to clarify how new insights can improve daily practice.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


