Effect of low-dose norepinephrine combined with goal-directed fluid therapy on postoperative pulmonary complications in lung surgery: A prospective randomized controlled trial
IF 5
2区 医学
Q1 ANESTHESIOLOGY
引用次数: 0
Abstract
Study objective
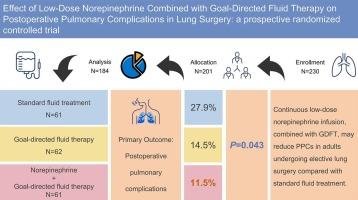
Postoperative pulmonary complications (PPCs), the predominant complications following lung surgery, are closely associated with intraoperative fluid therapy. This study investigates whether continuous low-dose norepinephrine infusion combined with goal-directed fluid therapy (GDFT) reduced the risk of PPCs after lung surgery relative to either GDFT alone or standard fluid treatment.
Design
A prospective, randomized controlled trial.
Setting
The First Affiliated Hospital of Anhui Medical University, Anhui, China.
Patients
The study included 184 patients undergoing elective thoracoscopic lung resection surgery.
Interventions
Patients were randomized into three groups based on different fluid treatment regimens: Group C received standard fluid treatment, Group G received GDFT, and Group N received continuous low-dose norepinephrine infusion combined with GDFT.
Measurements
The primary outcome was the incidence of PPCs, including respiratory infection, atelectasis, pneumothorax, pleural empyema, respiratory failure, pulmonary embolism and bronchopleural fistula, during the postoperative hospital stay. Secondary outcomes were hemodynamic variables and arterial blood gases. Additional recorded parameters included other postoperative complications such as bleeding, postoperative re-intubation, re-hospitalization within 30 days, and the length of hospital stay.
Main results
Group N showed a significantly lower PPCs incidence during hospitalization compared to Group C (11.5 % vs 27.9 %; odds ratio, 2.98; 95 % confidence interval, 1.17–8.31; P = 0.023). No significant difference in PPCs was found between Group N and Group G (11.5 % vs 14.5 %; odds ratio, 1.31; 95 % confidence interval, 0.46–3.91; P = 0.616). Additionally, there were no significant differences among the three groups in the components of PPCs. Group N showed higher mean arterial pressure and stroke volume index intraoperatively compared to Group C.
Conclusions
Continuous low-dose norepinephrine infusion combined with GDFT reduced PPCs incidence in elective lung surgery patients compared with standard fluid management, but showed no difference compared to GDFT alone.
Clinical trial registration
ChiCTR2200064081.
小剂量去甲肾上腺素联合目标导向液体疗法对肺部手术术后肺部并发症的影响:前瞻性随机对照试验。
研究目的:术后肺部并发症(PPCs)是肺部手术后的主要并发症,与术中输液治疗密切相关。本研究探讨了持续低剂量去甲肾上腺素输注结合目标导向液体疗法(GDFT)是否比单独使用目标导向液体疗法或标准液体疗法降低了肺部手术后肺部并发症的风险:前瞻性随机对照试验:地点:中国安徽省安徽医科大学第一附属医院:研究纳入了 184 名接受选择性胸腔镜肺切除手术的患者:根据不同的输液治疗方案将患者随机分为三组:C组接受标准液体治疗,G组接受GDFT治疗,N组接受持续低剂量去甲肾上腺素输注联合GDFT治疗:主要结果是术后住院期间 PPCs 的发生率,包括呼吸道感染、肺不张、气胸、胸膜腔积液、呼吸衰竭、肺栓塞和支气管胸膜瘘。次要结果是血液动力学变量和动脉血气。其他记录参数包括其他术后并发症,如出血、术后再次插管、30 天内再次住院以及住院时间:主要结果:与 C 组相比,N 组住院期间的 PPCs 发生率明显较低(11.5% vs 27.9%;几率比,2.98;95% 置信区间,1.17-8.31;P = 0.023)。N 组和 G 组的 PPCs 无明显差异(11.5% vs 14.5%;几率比 1.31;95% 置信区间 0.46-3.91;P = 0.616)。此外,三组在 PPCs 的组成成分方面没有明显差异。与 C 组相比,N 组在术中显示出更高的平均动脉压和每搏容积指数:结论:与标准液体管理相比,持续低剂量去甲肾上腺素输注联合 GDFT 降低了择期肺部手术患者的 PPCs 发生率,但与单独使用 GDFT 相比没有差异:临床试验注册:ChiCTR2200064081。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
7.40
自引率
4.50%
发文量
346
审稿时长
23 days
期刊介绍:
The Journal of Clinical Anesthesia (JCA) addresses all aspects of anesthesia practice, including anesthetic administration, pharmacokinetics, preoperative and postoperative considerations, coexisting disease and other complicating factors, cost issues, and similar concerns anesthesiologists contend with daily. Exceptionally high standards of presentation and accuracy are maintained.
The core of the journal is original contributions on subjects relevant to clinical practice, and rigorously peer-reviewed. Highly respected international experts have joined together to form the Editorial Board, sharing their years of experience and clinical expertise. Specialized section editors cover the various subspecialties within the field. To keep your practical clinical skills current, the journal bridges the gap between the laboratory and the clinical practice of anesthesiology and critical care to clarify how new insights can improve daily practice.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


