Unique cardiometabolic factors in women that contribute to modified cardiovascular disease risk
IF 4.7
3区 医学
Q1 PHARMACOLOGY & PHARMACY
引用次数: 0
Abstract
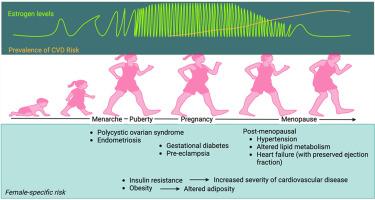
Major risk factors of cardiovascular disease (CVD) include hypertension, obesity, diabetes mellitus and metabolic syndrome; all of which are considered inflammatory conditions. Women are disproportionately affected by inflammatory conditions, with sex differences emerging as early as adolescence. Hormonal fluctuations associated with reproductive events such as menarche, pregnancy and menopause, are hypothesized to promote a pro-inflammatory state in women. Moreover, women who have experienced inflammatory-type conditions such as polycystic ovarian syndrome (PCOS), gestational diabetes or pre-eclampsia, have a cardiometabolic phenotype that pre-disposes to increased risk of myocardial infarction, stroke and coronary heart disease. Women with no notable CVD risk factors are often relatively protected from CVD pre-menopause; but overtake men in risk of major cardiovascular events when the cardiovascular protective effects of oestrogen begin to wane. Sex differences and female-specific factors have long been considered challenging to study and this has led to an underrepresentation of females in clinical trials and lack of female-specific data from pre-clinical studies. However, there is now a clear prerogative to include females at all stages of research, despite inherent complexities and potential variability in data. This review explores recent advancements in our understanding of CVD in women. We summarise the underlying factors unique to women that can promote CVD risk factors, ultimately contributing to CVD burden and the emerging therapies aimed to combat this.
导致心血管疾病风险改变的女性独特的心脏代谢因素。
心血管疾病(CVD)的主要风险因素包括高血压、肥胖、糖尿病和代谢综合征;所有这些都被认为是炎症。女性受炎症影响的比例更高,性别差异早在青春期就已出现。与月经初潮、怀孕和更年期等生殖事件相关的荷尔蒙波动被认为会促进女性的炎症状态。此外,经历过多囊卵巢综合症(PCOS)、妊娠糖尿病或先兆子痫等炎症型病症的女性,其心脏代谢表型容易导致心肌梗死、中风和冠心病的风险增加。没有明显心血管疾病风险因素的女性通常在绝经前受到相对保护,不会发生心血管疾病;但当雌激素对心血管的保护作用开始减弱时,发生重大心血管事件的风险就会超过男性。长期以来,性别差异和女性特异性因素一直被认为是研究的难点,这导致女性在临床试验中的代表性不足,临床前研究中也缺乏女性特异性数据。然而,尽管存在固有的复杂性和潜在的数据变异性,但目前在研究的各个阶段都有将女性纳入其中的明确特权。本综述探讨了我们对女性心血管疾病认识的最新进展。我们总结了女性特有的潜在因素,这些因素可促进心血管疾病风险因素的形成,最终导致心血管疾病负担,并总结了旨在解决这一问题的新兴疗法。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
9.00
自引率
0.00%
发文量
572
审稿时长
34 days
期刊介绍:
The European Journal of Pharmacology publishes research papers covering all aspects of experimental pharmacology with focus on the mechanism of action of structurally identified compounds affecting biological systems.
The scope includes:
Behavioural pharmacology
Neuropharmacology and analgesia
Cardiovascular pharmacology
Pulmonary, gastrointestinal and urogenital pharmacology
Endocrine pharmacology
Immunopharmacology and inflammation
Molecular and cellular pharmacology
Regenerative pharmacology
Biologicals and biotherapeutics
Translational pharmacology
Nutriceutical pharmacology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


