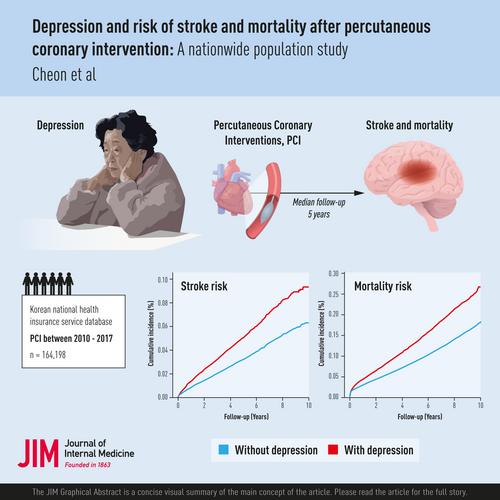
Depression and risk of stroke and mortality after percutaneous coronary intervention: A nationwide population study
Abstract
Background
Limited evidence exists on the role of depression in the risk of developing stroke and other cardiovascular outcomes in patients who have undergone percutaneous coronary interventions (PCI). We investigated this relationship with data from the Korean National Health Insurance Service database.
Methods
Our nationwide retrospective cohort study included 164,198 patients who had undergone PCI between 2010 and 2017. Depression was defined with the ICD-10 codes recorded prior to the PCI. The primary outcome was a new-onset stroke following the PCI. Secondary outcomes included PCI with myocardial infarction (MI), revascularization (PCI or coronary artery bypass grafting), and all-cause mortality. A multivariable Cox proportional hazards regression analysis was used to calculate adjusted hazard ratios (aHR) and 95% confidence intervals (CI), adjusting for potential confounders, including sociodemographic and lifestyle factors, comorbidities, and MI at the index PCI.
Results
Over a median follow-up of 5.0 years, acute stroke occurred in 5.7% of patients with pre-existing depression (17.4% of the study population), compared to 3.5% of those without depression. Depression was associated with a 27% increased risk of acute stroke (aHR 1.27, 95% CI 1.20–1.35). Additionally, depression was linked with a 25% elevated risk of all-cause death (aHR 1.25, 95% CI, 1.21–1.29) and an 8% increased risk of revascularization (aHR 1.08, 95% CI 1.04–1.11). The associations with the risk of stroke and all-cause mortality were stronger in patients under 65 years.
Conclusions
Our findings suggest that pre-existing depression may increase the risk of stroke and all-cause mortality following PCI, particularly in patients under 65 years. Additionally, depression was significantly associated with an increased need for revascularization. This underscores the potential benefits of managing depression to reduce stroke risk and overall cardiovascular outcomes following PCI.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


