Insulin resistance reduction, intermittent fasting, and human growth hormone: secondary analysis of a randomized trial
引用次数: 0
Abstract
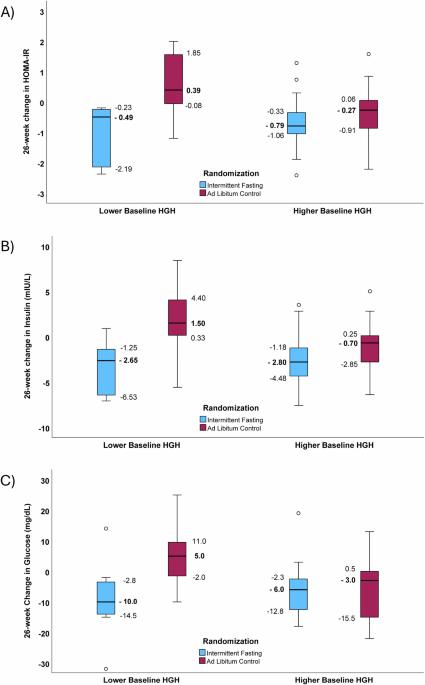
Intense intermittent fasting regimens safely reduce weight to a similar extent as caloric restriction. A previous trial reported low-frequency 26-week intermittent fasting reduced homeostatic model assessment of insulin resistance (HOMA-IR) without significant weight loss. During fasting, human growth hormone (HGH) increases substantially, but whether basal HGH modifies the effect of fasting on outcomes of repeated fasting is unknown. In a post hoc analysis of a randomized controlled trial (registration: clinicaltrials.gov, NCT02770313, May 12, 2016), subjects (N = 68) were adults ages 21–70 years with modest cholesterol elevation, ≥1 metabolic syndrome component, available HGH measurements, no chronic disease, and no statin or anti-diabetes medication. Randomization was 1:1 to intermittent fasting (24-hour, water-only, twice-per-week for 4 weeks, then once-per-week for 22 weeks) or 26-week ad libitum control. General linear modeling evaluated the interaction of trial arm with baseline HGH for HOMA-IR changes. Subjects with lower baseline HGH had 26-week HOMA-IR changes (p = 0.003) of −1.04 ± 0.99 for fasting versus 0.60 ± 1.04 for controls. Subjects with higher baseline HGH had HOMA-IR changes (p = 0.26) of −0.69 ± 0.75 (fasting) and −0.42 ± 0.92 (controls). The interaction of fasting with lower baseline HGH was significant (p-interaction=0.004). Results were similar for insulin and glucose. Weight loss at 26 weeks was not significantly different between fasting and controls (−1.74 ± 4.81 kg vs. 0.21 ± 3.50 kg, p = 0.08) and was not correlated with changes in HOMA-IR, insulin, glucose, and HGH. In conclusion, lower baseline HGH modified the effect of low-frequency water-only 24-hour fasting in profoundly reducing HOMA-IR over 26 weeks compared both to controls and to fasting subjects with higher baseline HGH.
减少胰岛素抵抗、间歇性禁食和人体生长激素:随机试验的二次分析
高强度间歇性禁食疗法能安全地减轻体重,其程度与热量限制相似。之前的一项试验报告称,为期26周的低频率间歇性禁食降低了胰岛素抵抗的稳态模型评估(HOMA-IR),但体重并未明显减轻。禁食期间,人体生长激素(HGH)会大幅增加,但基础 HGH 是否会改变禁食对重复禁食结果的影响尚不清楚。在一项随机对照试验(注册:clinicaltrials.gov,NCT02770313,2016年5月12日)的事后分析中,受试者(N = 68)为21-70岁的成年人,胆固醇适度升高,代谢综合征成分≥1个,有HGH测量值,无慢性疾病,未服用他汀类药物或抗糖尿病药物。按照 1:1 的比例随机分配到间歇性禁食(24 小时只喝水,每周两次,持续 4 周,然后每周一次,持续 22 周)或 26 周自由饮食对照组。一般线性模型评估了试验组与基线HGH对HOMA-IR变化的交互作用。基线HGH较低的受试者在26周的HOMA-IR变化(p = 0.003)为空腹-1.04 ± 0.99,而对照组为0.60 ± 1.04。基线HGH较高的受试者的HOMA-IR变化(p = 0.26)为-0.69 ± 0.75(空腹)和-0.42 ± 0.92(对照组)。空腹与较低基线 HGH 的交互作用显著(p-交互作用=0.004)。胰岛素和葡萄糖的结果类似。26周时,空腹与对照组的体重下降差异不大(-1.74 ± 4.81 kg vs. 0.21 ± 3.50 kg,p = 0.08),且与HOMA-IR、胰岛素、血糖和HGH的变化无关。总之,与对照组和基线HGH较高的禁食受试者相比,较低的基线HGH改变了低频纯水24小时禁食在26周内显著降低HOMA-IR的效果。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


